Moisture lesions and incontinence associated dermatitis
Download and print this article
DownloadPlease be aware that there are images of wounds on this page.
Introduction
This information is aimed at people who are at risk of developing a moisture lesion; people who have a moisture lesion; and carers.
This leaflet is to help you understand:
- What a moisture lesion is
- How to reduce the risk of developing a moisture lesion
- How to manage and treat a moisture lesion
This leaflet can be used in conjunction with our Pressure Injury patient and carer information leaflet.
What is a moisture lesion?
A moisture lesion is soreness and blistering where the skin has been exposed to wetness over a long period of time. This wetness can be urine, faeces, sweat or wound fluid.
Moisture lesions can vary in size, colour and shape. They often appear as patches of sore skin. The skin sometimes blisters and erosions form. They are often irregular in shape. It is common to find them in the skin folds and creases.
Moisture lesions are also known as ‘incontinence associated dermatitis’ and in children as ‘nappy rash’.

Mild moisture lesion
Moderate moisture lesion

Severe moisture lesion
How do I know if I have moisture lesion?
One of the first signs that you may have a moisture lesion is a feeling of wetness or irritation on the skin. If you feel wet or sore, it is important to let your nurse or carer know, especially if you need assistance with personal care.
The longer the skin is exposed to moisture, the more damaging it will be. It is important to keep the skin clean and dry to reduce the risk of developing a moisture lesion.
What are the risks of developing a moisture lesion?
Pain: Moisture lesions can be very painful because they are shallow wounds and nerve endings are exposed. However they are a minor skin condition and with good management and treatment should heal within 1-2 weeks.
Infection: Moisture lesions can increase the risk of infection. When moisture contains an irritant, like urine or faeces, it can damage the structure and function of the skin. The pH of urine is different to the pH of the skin, so when skin is exposed to urine for a prolonged period of time skin is weakened and some bacterial defences are reduced.
Faeces contain active enzymes that weaken the skin. Once the skin is damaged faecal bacteria are able to penetrate the skin, increasing the risk of infection. Bacteria also thrive in a warm and moist environment, so it is important to ensure the skin is clean and dry to reduce the risk of infection.
Pressure Injury: Having a moisture lesion can increase the risk of you developing a pressure ulcer. Also known as ’bed sores’, pressure injuries are areas of localised skin damage. They can occur anywhere on the body, but tend to occur on bony areas. The most common sites for pressure injury development are the bottom, hips, and the heels and elbows.
What causes a moisture lesion?
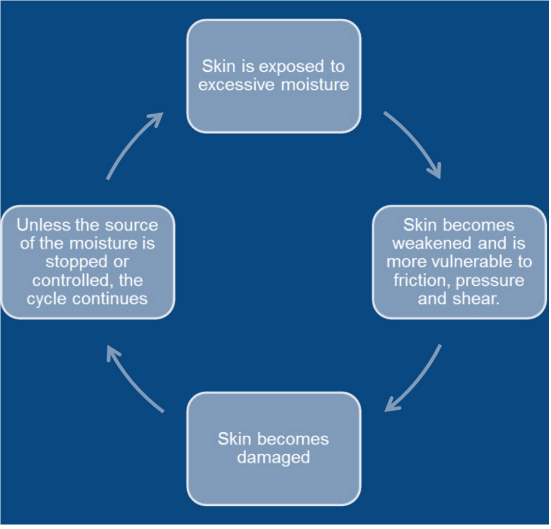
A moisture lesion is caused by exposure to excessive moisture for a long period of time. The four main causes are urinary incontinence, faecal incontinence, leaking wounds and excessive sweating.
Urinary incontinence is an involuntary passing of urine, meaning you pass urine when you do not mean to.
Faecal incontinence is an involuntary passing of faeces (poo), meaning you pass faeces when you do not mean to.
Leaky wounds can cause maceration (moisture damage) to the surrounding skin of the wound.
Excessive sweating can lead to a build up of moisture in the folds and creases of the skin.
How do I prevent a moisture lesion developing?
Managing Conditions
To prevent moisture lesions from developing, the condition that is causing the excessive moisture needs to be managed appropriately.
For example: if the moisture lesion is caused by diarrhoea, can it be treated? By treating the diarrhoea and stopping the source of moisture, the cycle is broken.
However not all these conditions can be treated, this is why good continence management, good skin care and effective wound management is essential. For more information and advice about how to manage any of these conditions, speak to your healthcare professional. One method to manage incontinence is the use of an
absorbent pad. These come in a variety of shapes and sizes to suit your needs.
Good Skin Care
Moisture lesions can be prevented through good skin care. There are four key steps to maintaining good skin care
- Cleanse: Wash vulnerable skin with either water or an emollient. Some soaps can be very harsh to skin and affect the lower pH levels of the skin.
- Dry: Dry skin with a gentle rubbing method. Pat drying has been found not to be effective. If skin is left moist, it is more vulnerable to damage. Talcum powder shouldn’t be used.
- Moisturise: Moisturise skin with an emollient (moisturising product), to help the skin stay supple and hydrated.
- Protect: Use a barrier product where the skin is exposed to excessive moisture to protect it from breaking down. Whilst you are in hospital, we will provide an appropriate barrier product to be used.
Good Nutrition and Hydration
Maintaining a healthy weight and good fluid intake helps to maintain good skin integrity. This can be achieved by eating a balanced diet and drinking at least 6-8 glasses of water a day.
Poor nutrition and hydration greatly impacts all wound healing by hindering tissue and skin repair.
If you notice you are eating and drinking less than you normally would, please inform your health care professional. You may need to be seen by a dietician and have extra nutritional supplements.
How do I need to do if I have a moisture lesion?
Manage the moisture
Managing the source of moisture is very important to allow the damaged skin to heal. If damaged skin is continually exposed to moisture, the damage is likely to get worse.
Good skin care
Follow the good skin care advice on the previous page. Cleanse, Dry, Moisturise and Protect.
Protect
Whilst you are in hospital we may use a barrier cream and/or a barrier film to protect your skin and wound from excessive moisture. This plan will be individualised to your needs and a product.
Effective repositioning
If you have a moisture lesion you will be more at risk of developing a pressure ulcer so you will be started on a repositioning regime, so you are not in the same position too long. You may find it frustrating to be turned and stood on a regular basis, but this is to ensure your safety whilst in hospital.
This regime can be discussed with your health care professional. Please see the Pressure Ulcer patient information leaflet for more advice.
Absorbent dressings
To manage very leaky wounds, a barrier film can be used alongside a highly absorbent wound dressing or wound manager bag to control the high volumes of wound fluid.
This information is intended for patients receiving care in Brighton & Hove or Haywards Heath.
The information here is for guidance purposes only and is in no way intended to replace professional clinical advice by a qualified practitioner.

