pressure ulcer prevention
Download and print as a PDF
DownloadPlease be aware that there are images of wounds on this page.
What are pressure ulcers?
Pressure ulcers are areas of damage to the skin and underlying tissue. They are also known as pressure sores or bed sores.
Pressure ulcers may cause pain or lead to an extended hospital stay. They can become infected, leading to blood poisoning or bone infection and in extreme cases can become life-threatening.
What causes pressure ulcers?
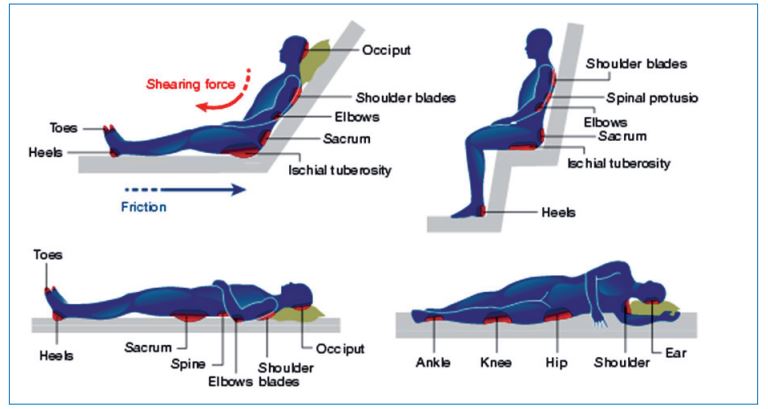
Pressure ulcers are caused by a combination of:
- Pressure – from body weight pressing against a hard surface, damaging the blood supply to that area
- Shearing – this may occur if you slide down, or are dragged up the bed or chair and may damage the deeper layers of the skin
- Friction – poor moving and handling techniques can remove the top layers of the skin
Common body sites for pressure ulcers are normally over bone prominence:
Are you at risk from pressure ulcers?
There are things we need to know to help prevent pressure ulcers from developing.
- Tell us if you’re not eating as much as you used to
- Tell us if you’re not moving as much as you used to
- Tell us if you have a sore bottom or heels, hips or elbows
- Tell us if you think there’s a problem with your cushion or mattress
- Tell us if you are sleeping in your chair rather than a bed
- Tell us you’re having incontinence problems
- Tell us if you have a reduced feeling in your feet
- Tell us if you have had a pressure ulcer in the past
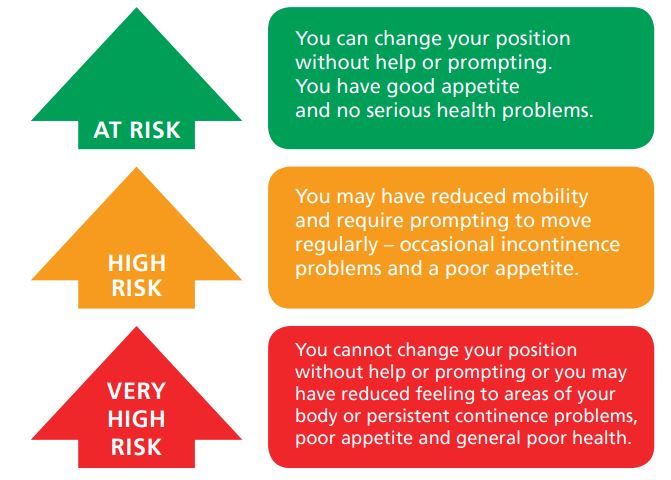
All the above increase the risk of developing a pressure ulcer and may move you from being ‘at risk’ through a ‘very high risk’.
Nutrition and hydration
Adequate nutrition and fluids are essential to prevent pressure ulcers. Please ask for advice if you are concerned.
What can you and your carer do to help prevent a pressure ulcer?
Regular skin inspections – your skin should be observed for:
- Purple/bluish patches on darker skin
- Red patches on lighter skin, that do not blanch following release of light finger pressure
- Swelling
- Blisters
- Shiny areas
- Dry patches, cracks or calluses.
Report any of these signs to the healthcare team looking after you.
Regular repositioning - If you can, change your position frequently.
- Please ask staff to assist you to do so, if you have difficulty changing position
- Make sure that bedding is crease free and not pulled too tightly across you, and that clothing does not have zips and buttons
- Make sure shoes/slippers and socks are not too tight as this will restrict your circulation. Please inform nursing staff if you feel any discomfort on this common pressure ulcers sites.
Use of equipment
A mattress or cushion may be provided that will help reduce the amount of pressure on your body. Please notify nursing staff if the equipment provided is not working or is uncomfortable. Water-filled gloves, synthetic and genuine sheepskins, and doughnut type devices should not be used. Equipment used for moving or lifting should not be left underneath you.
Inform nursing staff if you use any pressure reducing/relieving equipment in your usual care setting.

Example of the early stage of pressure ulcer development:

What happens if you develop/already have a pressure ulcer?
The Trust is committed to reduce the number of pressure injuries that develop whilst people are in our care. However, unfortunately due to the nature and severity of illness, pressure ulcers may still occur in a small number of people. If this happens appropriate preventive care will be provided and a wound dressing plan will be devised and implemented.
An investigation may also be cared out by the trust wound care specialist. You may require specialist equipment and input from community nurses on discharge.
If you need more information on pressure ulcer prevention and treatment, please ask the nursing staff on the ward and/or request a visit from the Tissue Viability Team.
This information is intended for patients receiving care in Brighton & Hove or Haywards Heath.
The information here is for guidance purposes only and is in no way intended to replace professional clinical advice by a qualified practitioner.
Publication Date: May 2019
Review Date: December 2022


