vulva cancer and vulval surgery
Download and print as a PDF
Download- What is the vulva?
- What is cancer of the vulva?
- Are there different types of cancer of the vulva?
- Are there any risk factors and/or causes of vulval cancer?
- What are the symptoms?
- How is cancer of the vulva diagnosed?
- How is my cancer graded and staged?
- How is cancer of the vulva treated?
- What can I expect before the operation?
- What are the risks and benefits of having vulval surgery?
- What can I expect after the operation?
- What about going home?
- Are there any alternatives to having a Vulvectomy?
- Who can I contact with any concerns or questions?
- References/useful links
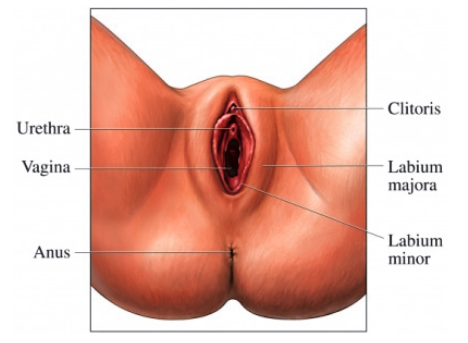
What is the vulva?
The vulva is the area of skin between a woman’s legs and makes up the outside part of the genital organs. It includes two outside lips (labia majora) typically covered in pubic hair and surround two
inner lips (labia minora).
The front of the vulva includes a small structure known as the clitoris, behind this is the urethra (the outlet for urine to pass) and further below is the vaginal opening.
The anus is not part of the vulva. In between the vaginal opening and anus is a smooth area of skin known as the perineum.
All of these areas are visible on the outside of the body.
What is cancer of the vulva?
Cancer is the uncontrolled growth of cells which are located in organs and tissues around the body. Normally cells divide themselves in an orderly controlled way, but sometimes this process can become out of control and the cells continue to divide developing a lump. This is also known as a tumour. Tumours can be either benign (non cancerous) or malignant (cancerous). Your doctor will be able to tell you whether the tumour is cancerous or not.
Cancer of the vulva is rare, on average 1,100 women are diagnosed with it each year in the UK. The majority of women are aged over 60, but an increasing number of younger women are now being diagnosed is on the increase continually. Vulval cancer can occur on any part of the vulva, but the inner edges of the labia majora and labia minora are the most common areas for it to develop.
Are there different types of cancer of the vulva?
Vulval cancers are normally categorised:
- Squamous Cell Carcinoma 9 out of 10 vulval cancers (90%) develop in the skin of the vulva from cells called squamous cells. This type of cancer usually takes years to develop and usually begins with pre cancerous changes to the vulval cells which over the years slowly change into cancerous cells
- Vulval Melanoma This is the second most common type of vulval cancer. 4 out of 100 vulval cancers (4%) are melanoma and they develop from the pigment producing cells which give our skin its colour. Vulval melanoma typically looks like a dark patch on the vulva
- Verrucous Carcinoma This is a rare slow growing squamous cell carcinoma that looks like a large wart
- Adenocarcinoma This again is very rare and develops from cells that line the glands in the vulva
- Basal Cell Carcinoma This type of cancer rarely affects the vulva. It develops from cells called basal cells which are found in the deep layer of the vulval skin. This is a slow growing cancer and almost never spreads anywhere else
- Sarcoma This is one of the rarest cancers and develops from the cells found in tissues such as muscle and fat. They tend to grow more quickly then other vulval cancers.
Are there any risk factors and/or causes of vulval cancer?
There are a number of factors associated with vulval cancer. These include:
- Age This risk develops with age, about 8 in 10 women (80%) who are diagnosed are over the age of 60
- Vulval skin conditions Women who suffer from non cancerous vulval skin conditions are at a higher risk of developing vulval cancer. The two main types are: vulval lichen sclerosus and vulval lichen planus. 3-5 / 100 women (3-5%) who have lichen sclerosus can develop vulval cancer over time
- Human Papilloma Virus (HPV) This is a very common infection usually passed during sexual intercourse. Most women with this infection do not have any problems as the body gets rid of the virus quickly, but in a number of women the virus remains and can lead on to abnormal changes in the vulva and surrounding skin
- Vulval Intraepithelial Neoplasia (VIN) A pre-cancerous condition that can occur in the skin surrounding the vulva. Though in some women VIN can develop into vulval cancer. There are two categories: VIN usual type and VIN differentiated. VIN usual is interlinked with HPV infection and majority of women affected are under the age of 50. VIN differentiated is interlinked with linchen sclerosus and generally affects women over the age of 50
- Smoking This increases a women’s risk of vulval cancer as smoking affects the way your immune system works and makes it less effective to fight infection. This could interlink with the HPV infection increasing chances of vulval cancer
- Pagets Disease A condition that causes abnormal changes to the cells that cover the skin around the vulva. This is rare and usually only affects women who have been through the menopause.
What are the symptoms?
You may experience some or all of these symptoms:
- Itching, burning or soreness of the vulva
- Lump, swelling or wart like growth of the vulva
- Red, white, dark patches on the skin of the vulva
- Thickened raised skin of the vulva
- Bleeding, or blood stained vaginal discharge not related to periods
- Pain when passing urine
- Tenderness or pain in the vulval area
- Sore or ulcerated area
- Mole on the vulva that changes shape or colour
Some of these symptoms occur due to other conditions and may not be cancer related.
Cancer of the vulva can take time to develop and like other cancers it is easier to treat/cure if diagnosed at an early stage.
How is cancer of the vulva diagnosed?
A range of tests and investigations may be carried out by your GP prior to them referring you onto a specialist (gynaecologist) although you may expect the following to occur:
- Vaginal Examination This is when the doctors examine your vulval area visually
- Biopsy This is known as the most reliable way to test for cancer and is where the doctor takes a small sample of the tissue from the abnormal area and sends to the laboratory to be examined under
the microscope - Blood tests this can include tests for your general health, see what levels your blood cells run at (full blood count) and check the liver and kidney function
- Chest X-Ray to see whether your lungs and heart are healthy
- MRI Scan this test uses magnetism for a more detailed picture of particular areas of your body
- PET Scan A test to see if the cancer has spread using glucose to measure the activity of cells in different parts of the body.
How is my cancer graded and staged?
Your cancer will be graded like other cancers and this will aid your doctor to know what the most appropriate treatment is for you. Grading usually happens from biopsies and they refer to the appearance of cells underneath the microscope.
- Grade 1 (Low) The cancer looks like normal cells of the vulva growing slowly
- Grade 2 (Moderate) The cells look more abnormal then grade 1 but not as abnormal then grade 3
- Grade 3 (High) The cells look very abnormal. They grow very quickly and more likely to spread.
Staging is a term used to describe the cancer size and whether it has spread beyond where it had initially started.
The commonly used system for staging is below:
- Stage 1 The cancer is localised in the vulva and/or perineum only
- Stage 2 The cancer is any size and has spread to nearby areas (urethra, vagina and/or anus)
- Stage 3 The cancer has spread into the lymph nodes located on either side of your groin
- Stage 4 The cancer has spread to the lymph nodes in the pelvis and/or other areas of the body further away.
How is cancer of the vulva treated?
An operation is the main treatment for vulval cancer.
The different types of operations are:
- Radical Wide Local Excision
Removing the cancer and a border (margin) of healthy tissue surrounding the cancer usually about 1cm - Radical Partial Vulvectomy
Part of the vulva is removed. How this operation is done depends on where your cancer is. Your doctor will discuss this more with you - Radical Vulvectomy
The entire vulva is removed, including the inner and outer labia and clitoris. - Lymph Node Dissection
Lymph nodes are situated in your groin on both sides. Your doctor will tell you if these will be removed and from what side. This may be done at the time of the initial operation or may be arranged at a later date once the operation site has settled down after removal of the primary tumour.
Many women can be cured by having an operation, but sometimes the operation needs to be used in combination of other treatment – radiotherapy and/or chemotherapy. This will be discussed with you.
Your treatment plan will be made specifically to your health and well being and will include a team of specialists: gynaecologist oncologist, clinical oncologist, radiologist and a specialist nurse.
What can I expect before the operation?
At your pre-operative assessment and on your admission day the nurse will go through the hospital stay and explain your operation. Please do let us know about any concerns you have or any information you think we should know about, that will make your stay with us more comfortable.
You will need to make arrangements for your family, children or any other commitments that you have prior to coming in to hospital and to cover the length of your recovery. On arrival you will see an anaesthetist and the doctor performing the operation before you go to theatre. It is not unusual to feel anxious; the nursing staff will gladly discuss with you how you feel and talk through your emotions.
On the day of your admission please do not eat anything 6 hours before your admission time this includes sweets and chewing gum. Drink water only for 2 hours before your admission time.
Please note the following:
- If you are a smoker we strongly recommend that you do not smoke at all on the day before and the morning of your operation or for 48 hours after your operation
- Please bring in with you any medication that you usually take in the original packaging
- Do not bring in valuables or money except for some change for the Patientline TV and phone
- Do not wear make-up, nail varnish or jewellery
- Please remove your contact lenses.
What are the risks and benefits of having vulval surgery?
The benefit of your operation is to remove the cancer. There are risks with any operation but these are small.
The main risks associated with undergoing a vulval procedure are:
- Pain
- Urinary infection, inability to pass urine and/or frequency
- Wound infection, bruising and delayed wound healing
- Excessive bleeding
- Venous thrombosis and pulmonary embolism (blood clot in leg/lung)
- Lymphocyst – A collection of lymph fluid in the groin
- Lymphoedema
- Adverse reaction to the anaesthetic.
What can I expect after the operation?
After having a general anaesthetic you may experience episodes of pain and/or nausea – this is very common. Please let the nursing staff know and they will assess you and take appropriate action.
We use a pain score to assess your pain
0-10; 0 = No Pain, 10 = Very Strong Pain
Your nurse will be checking your blood pressure, pulse, breathing and temperature and monitoring the vulval area/wound for any oozing and or bleeding. S/he will also ask you to move from side to side and to do leg and breathing exercises once you are able, this will help prevent any pressure damage, a DVT (deep vein thrombosis) or chest infection.
The type of care you receive and the speed of your recovery will depend on the operation you have had.
The first 24 hours after the operation
You will have a drip attached in your arm (intravenous infusion); once you are fully awake you will be able to start drinking and eating. Your drip will then be discontinued.
You may have a catheter which will drain urine from your bladder. If not the nursing staff will help you mobilise out to the toilet.
You may also have one or even two drains in the groin to drain lymph fluid from your wound sites. This will be measured on return to the ward and then on a daily basis and a decision will be made by the doctors when they can be removed.
The nursing staff will assist with washing and dressing as necessary. Vulval hygiene (keeping the area clean) will be encouraged and taught on the ward for you to continue with. This should be carried out 2-3 times daily and involves the area being gently rinsed with water, most commonly by doing so in the shower or by using a jug of warm water. This will promote good wound healing and minimise risks of infections.
If your operation has involved the lower (posterior) section of your vulva, the doctors and nursing staff may ask you to avoid sitting and suggest standing and lying only. This is for your comfort reasons and promotes wound healing. Ask if you are unsure if this applies to you.
What about going home?
Each day you will be assessed by nursing and medical staff to check on your recovery and decisions will be made about your care, this information will of course be shared with you.
The average length of stay following vulval surgery can be from 1 to 5 days. As you physically recover from your operation the nursing team will discuss your convalescence. To ensure you have a good recovery you should note the following:
Wound Care:
We recommend you visit the practice nurse regularly for wound checks. If you are unable to do so let the nursing staff know prior to going home and a district nurse referral will be made.
Stitches:
Your wound will be closed by stitches which are usually dissolvable over 4-6 weeks.
Hygiene:
We emphasise that you shower daily. You should be washing/rinsing the vaginal area and wound with
clean fresh water up to 3 times per day either in the shower or by using a jug of warm water over the toilet. Maintaining strict high standards of vulval hygiene as taught on the ward will promote good wound healing and prevent infections.
Bleeding/Discharge:
Due to the internal healing process you may experience some minor vaginal bleeding. Your wound may ooze, bleed or have some discharge which can be offensive in odour. Make sure you wear sanitary pads, changing these regularly for hygiene reasons. If these symptoms worsen and you have an increase in discharge, worsening odour or the wound begins to open you must notify your GP or alternatively the Gynaecology Assessment Unit (GAU) located on Level 11 at the hospital.
Lymphocysts
You may notice that after the drain/s have been removed the groin area becomes painful, red, hot to touch and you may notice fluid leaking. If you are at home and you experience these symptoms you must contact the gynaecology ward as soon as possible.
Sometimes the collection of fluid that has built up needs draining and a small incision is made by the doctor to let this out. If this happens we would provide you with drainage bags (also known as stoma bags) to place over the incisions and keep the fluid draining.
If this happens you should write down the product code so if you need a repeat prescription for more bags your GP will be able to order them.
Product Code ____________________
It would be advisable that you monitor how much you are emptying from your drainage bags so that you can inform the doctors at your next outpatient appointment.
Rest:
During the first two weeks at home it is common to feel tired and exhausted, you should relax during the day gradually increasing the number of things you do each day. Avoid crossing your legs when you are lying down.
Housework:
We recommend that you do light activities around the house gradually introduce lighter household chores, dusting, washing up, making beds and ironing.
Exercise:
Exercise is important and it is advisable to go for short walks each day, increasing the distance gradually. You may return to normal exercise such as cycling and swimming after 6 weeks. You will be able to manage the stairs on your arrival home.
Diet:
A well balanced nutritious diet with high fibre content is essential to avoid constipation. Your bowels may take some time to return to normal after your operation and you will need to take laxatives. You should include at least 5 portions of fruit and vegetables per day. You should aim to drink at least 2 litres of water per day.
Sex:
You should wait for 6 weeks or when you feel comfortable to ensure that you are fully healed.
Driving:
It is usually safe to drive after 4-6 weeks but this will depend on your level of concentration, ability to perform an emergency stop, your insurance cover and comfort.
Are there any alternatives to having a Vulvectomy?
Your doctor should explain all alternatives to you prior to having the proposed procedure and explain why that chosen option is necessary letting you have an open and informed choice regarding your care and management.
Who can I contact with any concerns or questions?
If you have any problems or are worried, please do not hesitate to contact us on the gynaecology ward:
Royal Sussex County Hospital Level 11 Telephone: 01273 523191
Princess Royal Hospital Horsted Keynes Telephone: 01444 441881 Ext. 5686
References/useful links
Macmillan Cancer Support.
www.macmillan.org.uk
Telephone: 0808 8080 000
References/useful links
Macmillan Cancer Support
www.macmillan.org.uk
Tel: 0808 8080 000
Patient.co.uk Vulval Cancer Leaflet
This information is intended for patients receiving care in Brighton & Hove or Haywards Heath.
The information here is for guidance purposes only and is in no way intended to replace professional clinical advice by a qualified practitioner.
Publication Date: February 2018
Review Date: October 2022

