Stress incontinence of urine
Download and print as a PDF
DownloadWhat is stress incontinence of urine?
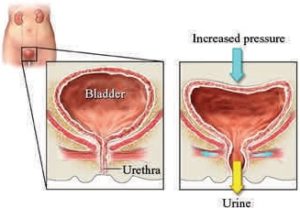
Stress incontinence of urine is involuntary leakage of small drops of urine on coughing, sneezing, exercise or movement.
The condition can cause considerable distress to patients and an affect their quality of life. The fear of having to go to the toilet quickly makes patients look out for toilets all the time. This limits activity and leads to isolation.
Stress incontinence of urine
What causes stress incontinence of urine?
Stress incontinence of urine is caused by weak support to the bladder neck, which is the area between the bladder and the urethra, as illustrated above.
This weakness can result from a number of factors, including;
- Pregnancy and delivery.
- Drop of female hormones after the menopause.
- Inherent weakness of the ligaments, which can be associated with joint hypermobility (wide range of movement).
The weakness can be exposed by;
- Heavy lifting and straining.
- Smoking.
- Being overweight.
These are the same factors that can cause pelvic organ prolapse (slipping down of the vagina and / or uterus) and the two conditions often co-exist.
How is the diagnosis made?
The diagnosis is helped by completing a bladder diary (Frequency Volume Chart). Examination is usually carried out to detect other problems, such neurological disease or pelvic organ prolapse. You might be asked to cough to see if you leak urine, but this is not a requirement for the diagnosis.
A sample of urine might be checked for infection and an ultrasound scan might be carried out to check that you empty your bladder fully.
Investigations to detect the problem include urodynamics. This is a test that assesses the function of the bladder by filling it using a catheter and checking for leakage on coughing and sneezing.
The tests are carried out in those patients who do not respond to conservative measures, especially those who have a combination of stress incontinence and overactive bladder, which manifests in the form of frequency and / or urgency of micturition and / or urge incontinence.
How is the condition treated?
Co existing problems, such as pelvic organ prolapse and / or uterus may modify the management. In the absence of such problems, treatment is primarily conservative, resorting to surgery upon failure of conservative measures.
Conservative measures include:
Fluid advice: Try to drink a normal amount of fluid. Not drinking enough may irritate the bladder. Drinking too much may cause distension of the bladder.
For the climate in the UK, an average person is expected to drink 24ml/kg/day, which equates to about 1.5 to 2 litres (about 7 mugs or 10 cups) per day. Avoiding irritants, such as caffeine, alcohol, fizzy drinks and acidic juices will reduce irritation of the bladder.
Pelvic floor muscle training:Guidance by a specialist physiotherapist is important, as up to a third of patients may not contract their pelvic floor muscles properly. A specialist physiotherapist will also guide you in getting to contract pelvic floor muscles before sudden stress, such as sneezing, which is known as the knack.
Pelvic floor muscle training requires daily perseverance over a minimum of 4 months to show an effect.
Medication: A tablet is available to reduce stress incontinence but can cause nausea. Local hormone replacement therapy in form of oestrogen cream or pessary may be tried in patients with atrophy (thinning) of the vagina (front passage) after the change.
Surgery
- Autologous sling: an operation to support the urethra using a strip from the abdominal (tummy) wall.
- Colposuspension: an operation to support the area around the bladder neck to the back of the bone in the lower tummy. This can be done open or laparoscopic (key hole).
- Injection of urethral bulking agent: an operation to support the bladder neck by injecting synthetic material.
The use of the tension free vaginal tape (TVT) sling was paused in 2017, due to concerns about safety.
What can I do to support the treatment?
- Stopping smoking helps avoiding coughing and also reduces bladder irritation. This can be difficult and the NHS smoking cessation help line can help in this respect.
- Weight loss and avoidance of constipation will reduce the pressure in the abdomen, which in turn will reduce the instances of leakage.
- Referral to a dietician can be arranged if required.
Those who do not get adequate improvement on these conservative measures are offered surgery.
Who can I contact with any concerns or questions?
Who can I contact with any concerns or questions? You should contact your GP or the hospital if you notice increased temperature, wound swelling and / or pain, smelling discharge either from the wound or the front passage, blood in urine or motion, abdominal distension and / or failure to open your bowel.
If you have any problems or questions, please use the telephone numbers to speak to one of the urogynaecological team.
Princess Royal Hospital: 01444 441881 Extension 5686
Royal Sussex County Hospital: 01273 696955 Extension 4013
Urogynaecology Unit at Lewes Victoria Hospital: 01273 474153 Extension 2178
Useful links:
This patient information leaflet was prepared by Dr. Sharif Ismail, Consultant Subspecialist Urogynaecologist.
This information leaflet has been approved at the Clinical Governance and Safety and Quality Meetings of the Department of Obstetrics and Gynaecology as well as Brighton and Sussex University Hospitals NHS Trust Carer and Patient Information Group (CPIG).
Ratified April 2017 Women’s Safety and Quality Committee.
This information is intended for patients receiving care in Brighton & Hove or Haywards Heath.
The information in this leaflet is for guidance purposes only and is in no way intended to replace professional clinical advice by a qualified practitioner.
Publication Date: May 2021
Review Date: February 2024


