Skin graft and donor site
Download and print as a PDF
DownloadPlease be aware that there are images of wounds on this page
- Why do I need a skin graft?
- What is a split skin graph (SSG)?
- Why should I have a SSG?
- What are the benefits of having a skin graft?
- Caring for graft
- What will the graft look like?
- Risks associated with a split thickness skin graft (SSG): SSG failure (partial or complete)
- Factors that can affect graft survival include:
- Donor sites
- Care of your dressings / wound
- Who can I contact for further information and advice?
Why do I need a skin graft?
A skin graft is to replace damaged skin (tissue). You may need to have a skin graft if you have suffered a burn, trauma or need plastic reconstructive surgery.
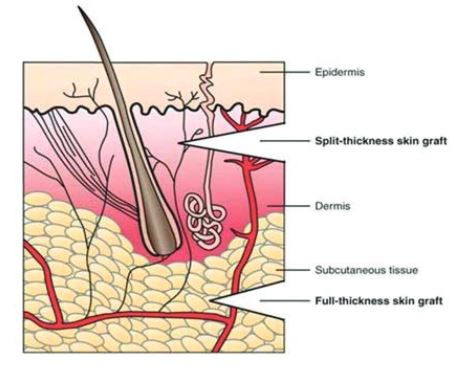
What is a split skin graph (SSG)?
Why should I have a SSG?
In some cases a wound is too large or too tight to be able to bring the edges together for direct closure. In these cases a SSG is an effective way of closing a wound. Although SSGs will take a few weeks to heal this time is much less than if the wound was left to heal without any intervention.
What are the benefits of having a skin graft?
- Help to heal the area quicker.
- Help reduce pain and discomfort when dressing changed.
- Help to reduce the risk of infection.
- Help reduce the chance of scarring.
- Cover an area that has lost skin.
Caring for graft
- Clean and free from infection.
- Avoid stretching or moving around the graft area, or affected limb unless you are told otherwise by medical staff or physiotherapist.
- The graft will have a firm dressing in place to stop friction or movement.
- The grafted area must be raised when sitting and if the graft is on a leg you should avoid standing for long periods of time.
- Daily activities should be increased gradually over two to three weeks.
- The pressure of the dressing will stop fluid collecting under the new skin. The dressing is usually left over the graft for 3 days, and will then be looked at by a doctor or nurse.
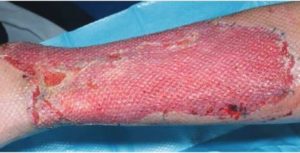
What will the graft look like?
Risks associated with a split thickness skin graft (SSG): SSG failure (partial or complete)
Skin grafts do not take their own blood supply with them, they need a healthy wound bed that can grow into them and give them a blood supply. As this happens, the skin graft starts to stick down to its new bed and gradually becomes incorporated into the surrounding skin. This is called the process of skin graft ‘take’.
Sometimes this is not possible because the wound bed that the SSG has been placed on is not healthy and, therefore, the graft does not survive.
Factors that can affect graft survival include:
- Infection: If the wound bed and graft become infected some or all of the graft may not survive. If this is the case you may need antibiotics, prolonged dressings or further surgery.
- Collection of fluid underneath the graft: If a collection of fluid lifts the graft off its bed then it is not able to get a new blood supply from it and so can’t survive. This collection of fluid can either be blood or seroma (straw-coloured fluid).
- Movement (shear): If the graft moves around too much on its new wound bed, the graft is not able to stick in place and get a new blood supply. To stop the graft moving around, you will have secure dressings in place as discussed above. We usually have a look at the graft after 5 days, at which point we know whether the graft has been successful.
- Inappropriate wound bed: Sometimes if the wound bed is not ready, the graft may not be able to survive. In this case, you may need a further operation or different type of operation.
- Smoking: Smoking affects all types of wound healing and the survival of your skin graft is no exception. Smoking makes the very tiny blood vessels in your body less efficient at transporting blood to and from an area and so it may mean that your skin graft may not survive.
- Poor nutrition: Wound healing, including your skin graft, may be affected by lack of vitamins and nutrients. If this is the case, we may get a dietitian to see you, to help improve the situation.
- Diabetes: If you have poorly controlled diabetes this may affect your ability to heal and so we will try and optimise your control before considering a skin graft.
Donor sites

Care of your dressings / wound

Once the top two dressings have been removed, you should then wash over the white dressing every day with soap and water. Pat off excess moisture and leave open to the air to dry. Do not be tempted to cover the white dressing tempted to cover the white dressing.
If the area still oozes fluid, step up the washing to two or three times a day. This will help to get rid of any excess fluid and the white dressing will eventually dry.
As the edges start to lift off these should be trimmed back to prevent catching on your bedding and clothes.
If the wound starts to smell or the surrounding skin starts to become red and painful. Increase the washing to night and morning. If this doesn’t improve contact the Plastic team.

Once the area has healed fully the white dressing will fall off. This can take up to six weeks.
Once healed, the area may appear dry. You can use a non-perfumed moisturiser two to three times a day to help keep the area soft.

Who can I contact for further information and advice?
For further information and advice please email the Plastic Surgery team: uhsussex.plasticsteam@nhs.net
This information is intended for patients receiving care in Brighton & Hove or Haywards Heath.
The information in this leaflet is for guidance purposes only and is no way intended to replace professional clinical advice by a qualified practitioner.
Publication Date: May 2021
Review Date: February 2024


