Pelvic organ prolapse
Download and print as a PDF
DownloadWhat is pelvic organ prolapse?
Pelvic organ prolapse means slipping down of the vagina and / or uterus. Prolapse (slipping down) can affect the front and / or back walls of the vagina and / or the uterus or the vaginal vault (top of the front passage after removal of the uterus).
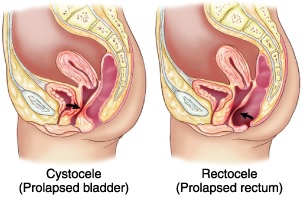
Prolapsed bladder and prolapsed rectum
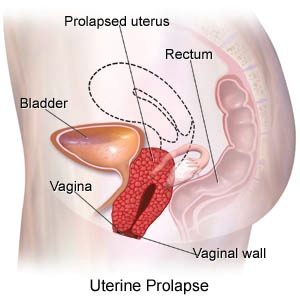
Uterine prolapse
What causes pelvic organ prolapse?
Pelvic organ prolapse is the result of weakness of the ligaments and muscles that support the vagina and uterus in their normal place. This weakness can result from a number of factors, including pregnancy and child bearing, heavy lifting and straining, going through the menopause as well as inherent weakness of the ligaments and muscles, which can be associated with joint hypermobility. The same applies to stress incontinence of urine, which may co exist with pelvic organ prolapse.
What are the effects of pelvic organ prolapse?
Not all patients having pelvic organ prolapse have problems. If problems occur, they do not necessarily reflect the degree of prolapse. Some patients have significant bother with minimal degree of prolapse while others have little to note with major degrees of prolapse.
Common symptoms include;
- Sense of bulge or lump down below.
- Dragging sensation, especially towards the end of the day.
- Urinary problems, like stress incontinence (leakage of urine on coughing and sneezing), frequency and / or urgency of micturition as well as difficulty passing urine. Some patients can not pass urine without pushing the prolapse up.
- Bowel symptoms, which may include the need to push prolapse to open the bowel.
- Difficulty with sexual intercourse.
How is this condition diagnosed?
Prolapse is confirmed after an internal examination which is usually carried out while lying on the back and on the left side. In difficult cases, patients might be examined while standing up and sometimes examination under anaesthesia might be necessary to establish the extent of pelvic organ prolapse.
How is the condition treated?
If prolapse is not causing any problems, it is left alone. If it is causing problems, then treatment is offered in the form of a vaginal pessary or surgery.
Weight loss, reduction or avoidance of straining and heavy lifting, addressing constipation, smoking cessation and the local oestrogen, or alternative preparation, are helpful measures.
Pelvic floor muscle training:
This can help mild pelvic organ prolapse and may help moderate pelvic organ prolapse. Pelvic floor exercises are good to perform. A physiotherapist can guide performing exercises better.
Vaginal pessaries:
These control, rather than cure, prolapse though many patients get symptom relief with them. Commonly used types are the ring, shelf and Gellhorn pessaries. Patients can have sex whilst using a ring pessary but not whilst using a shelf or a Gellhorm pessary. Fitting a pessary for the first time is a matter of trial and error and it can take a few goes to find the right size and shape.
Pessaries are usually offered to patients who can not have surgery for medical reasons or those who wish to defer surgery for some time, for example to have more children. There is a special information leaflet on the use of vaginal pessaries for pelvic organ prolapse.
They need to be replaced every 6 months to avoid ulceration of the vagina. You can replace the vaginal ring pessaries yourself. This option gives you the freedom to change vaginal ring pessaries when you like, for example by night or before sex. As long as you change the vaginal ring pessary at least once every six months, then you only need to see a nurse or a doctor every two years. This will reduce the need to attend in General Practice or at the Hospital. There is a special information leaflet on self management of vaginal ring pessaries.
Surgery:
A number of surgical procedures can be performed to correct pelvic organ prolapse and the choice depends on the type and extent of prolapse as well as your age and future fertility plans. In most cases, a vaginal repair is adequate. The uterus may be removed vaginally at the same time, unless you wish to keep it, for example to have more children, in which case it can be supported strongly to one of the ligaments. Patients with prolapse of the vaginal vault (top of the vagina after removal of the uterus) may have operations carried out through the vagina, abdomen or laparoscopic to support the top of the front passage. There is a special information leaflet on each of these operations.
Who can I contact with any concerns or questions?
If you have any problems or questions, you can contact:
Princess Royal Hospital, Horsted Keynes Ward: 01444 441881 Extension 5686
Royal Sussex County Hospital, Level 11: 01273 523191 Extension 4013
Urogynaecology Unit at Lewes Victoria Hospital: 01273 474153 Extension 2178
References and useful links:
Web MD website: Pelvic Organ Prolapse
This patient information leaflet was prepared by Dr. Sharif Ismail, Consultant Subspecialist Urogynaecologist.
This information leaflet has been approved at the Clinical Governance and Safety and Quality Meetings of the Department of Obstetrics and Gynaecology as well as Brighton and Sussex University Hospitals NHS Trust Carer and Patient Information Group (CPIG).
Ratified April 2017 Women’s Safety and Quality Committee.
This information is intended for patients receiving care in Brighton & Hove or Haywards Heath.
Disclaimer
The information in this leaflet is for guidance purposes only and is in no way intended to replace professional clinical advice by a qualified practitioner.
Publication Date: May 2021
Review Date: February 2024


