Open fractures
Download and print as a PDF
DownloadPlease be aware that there are images of wounds on this page
- What this guide tells you about
- What is an open fracture and what are the potential complications?
- How do you treat an open fracture?
- Orthopaedic Surgery (Fixing the Bone): How will my bone be fixed?
- What is external fixation?
- What is internal fixation?
- Plastic Surgery Soft Tissue Reconstruction: Why am I having a Soft Tissue Reconstruction?
- What types of Soft Tissue Reconstruction are there?
- How will my Soft Tissue Reconstruction change over time?
- What happens after my surgery?
- How long will I be in the hospital?
- Will I have pain?
- Will I have pain when I am home?
- How can I prevent muscle wastage?
- How can I prevent constipation?
- When will my stitches be removed?
- How do I look after my donor site?
- How do I care for my incisions?
- When can I shower?
- When can I swim?
- When can I resume my normal activities?
- When is it safe for me to drive?
- When can I exercise?
- When can I resume sexual activity?
- What type of follow-up care will I receive after I leave the hospital?
- How can I cope with my feelings?
- What if I have other questions?
What this guide tells you about
1. Your orthopaedic surgery (fixing the bone)
2. Your plastic surgery (soft tissue reconstruction)
3. What to expect after your surgery
4. Commonly asked questions.
What is an open fracture and what are the potential complications?
An open fracture is a broken bone that has come through the skin. They are typically caused by high-energy injuries such as road traffic collisions, falls or sports injuries. Urgent treatment is required as open fractures are at much greater risk of infection, and delayed healing of the bone, compared to fractures with intact skin. Bone infection can be difficult to treat and in a worst-case scenario, amputation of the limb might be required, although this is unusual.
How do you treat an open fracture?
As the skin over the fracture has been broken, infection can spread easily to the fracture site. Patients with open fractures require urgent surgery performed by orthopaedic and plastics surgeons working together to remove any debris, clean the wound and remove any unhealthy tissue.
This is known as debridement and often leads to a larger wound in the skin. Debridement is crucial as any dead tissue or bone left in the wound can lead to infection. Antibiotics and a tetanus booster are given at the same time.
After the debridement is complete, and if the wound can be closed (stitched together), the bone can be fixed together internally (internal fixation).
If internal fixation doesn’t work, you will be fixed together externally as a temporary measure (external fixation), and the wound will be covered, usually with a suction dressing (picture below). You will then return to theatre in the next few days for final bone fixation by the orthopaedic surgeon and soft tissue reconstruction by the plastic surgeon in a joint operation.

Suction dressing
You will meet with the Orthopaedic and Plastic Surgery Team before the operation. They will make sure it is safe for you to have surgery and will be happy to answer any questions you may have. The surgeons participating in this operation will be highly trained professionals, who have years of experience and have been involved in a lot of these kind of operations before.
You may also have:
- Photographs taken of your soft tissue wound that will be used during the reconstruction, as well as for comparison before and after your operation. These pictures are only taken with your informed consent; do not include your face; are managed confidentially; and are kept in your notes and/or into a secure BSUH NHS Trust computer server.
- Scans that use special dye (angiograms), such as CT or MRI, may be used to evaluate the blood vessels that supply your limb(s) and help with operative planning
Orthopaedic Surgery (Fixing the Bone): How will my bone be fixed?
Open fractures almost always need surgery to put the bone back and hold it there while it heals. This can be done in a number of ways. Examples are shown below. Your surgeon will discuss with you what he/she feels is in your best interest.
What is external fixation?
External fixation is when pins or wires into the bone are attached to rings or rods outside the limb. External fixators are used commonly as a temporary measure but can also be used as the final treatment and removed once the bone has healed.

External fixation of the bone
What is internal fixation?
Internal fixation is when either a rod inside the bone or plates on the surface of the bone are fixed to the bone with screws. These generally stay in forever but can be removed if there are any problems, but this is very uncommon.

Intramedullary nail or rod bony fixation

Plate and screws bony fixation
Plastic Surgery Soft Tissue Reconstruction: Why am I having a Soft Tissue Reconstruction?
In an open fracture there can be significant damage to, and loss of, the skin and muscle around the fracture. In order to reduce the risk of infection to the bone and metalwork, the wound must be closed when the bone is fixed. Unless it is a very small hole that can be closed, a soft tissue reconstruction is required. These operations are usually long (can take all day), and a general anaesthetic is most commonly used, unless otherwise advised from the Anaesthetic team.
What types of Soft Tissue Reconstruction are there?
Depending on the size and location of the wound, as well as the cause, the Plastic Surgery team may use:
- A skin graft: A very thin layer of skin, equivalent to a deep graze, usually taken from the upper thigh or buttocks. This tends to be used when the bone is still well covered with muscle.

Recently healed skin graft donor site on the thigh.
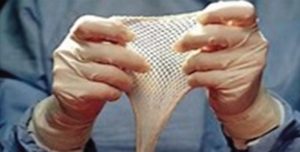
Meshed skin graft.
- A local flap: This method uses skin next to the wound, which is partially detached and rotated in order to cover the wound. This often creates a secondary skin defect which requires a simple skin graft, this is performed at the same time.

Skin and fat flap mobilised to cover wound on leg with secondary wound resurfaced with skin graft.
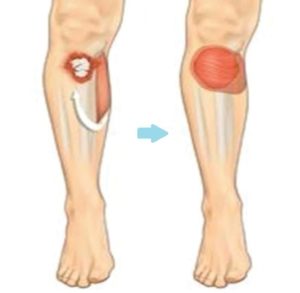
Calf muscle transferred to cover a wound at the front of the leg (picture from www.bapras.org.uk)

Diagram depicts a muscle taken from the thigh to cover a wound over
an open fracture on the other leg; the donor site is closed directly,
and the muscle flap is covered with a skin graft (picture from www.bapras.org.uk). - A distant ‘free’ flap: A block of tissue is taken, along with its blood vessels, from a distant part of your body (the donor site) and placed into the wound. This may be in a composite form, which is skin and fat or muscle, or may be just muscle. The blood vessels are then re-attached to the recipient site using microsurgical techniques and the transplanted tissue lives on its new location. The donor site is either stitched closed or may need to be resurfaced with a skin graft. Muscle flaps without skin also require a skin graft on top.
How will my Soft Tissue Reconstruction change over time?
Soft tissue reconstruction, especially involving muscle, always looks bit bulky at start.
However, as the flap matures over time, its volume reduces. It usually levels with the tissue around it but can sometimes remain a bit bulky.
The colour of the flap changes over time to more or less match the skin next to it. The size and colour change is a process that takes time to settle, usually 9-12 months.
The pictures below show a timeline of a muscle flap immediately after the operation (left), after 3 months (right), and after 9 months (bottom).
Very occasionally, any bulkiness that remains can be treated, if necessary, with secondary procedures.

Muscle flap day 1 after operation

Muscle flap 3 months after the operation.

Muscle flap 6 months after the operation.

A skin and flap day 1 after surgery.

A skin and fat flap 4 months after surgery.
What happens after my surgery?
- For the first few days, you will need to remain on bed rest and keep your injured limb elevated on pillows to reduce the swelling and keep a healthy blood flow to your limb.
- Your flap will be monitored closely by the ward nurses who will monitor the blood flow in and out of the flap, using a non-invasive machine, called a Doppler.
- It is important that you are kept warm for up to 48 hours after surgery to ensure that the blood flow in and out of the flap is maintained. You may also have a catheter (tube into your bladder) in place following surgery so that the surgical team can monitor your urine output.
- You will have your temperature, blood pressure and pulse checked regularly, and you will be given fluids through an intravenous drip (into your vein). You may have a wound dressing around the flap, with a clear window to allow the nurses to monitor the flap.
- After approximately three to five days, the wound dressing will be removed, and the flap left exposed. Following flap surgery, you will have a donor site, where the flap has been taken from and this will have a dressing in place. This will be removed at the time of your first flap inspection.
- On approximately day five, you can start to ‘dangle’ your limb (lower the limb over the side of the bed) for short periods of time and the physiotherapists and nurses will explain and advise you on this movement.
- On day seven, you can usually start to mobilise with the help of physiotherapy and a possible walking aid (such as crutches or a frame).
How long will I be in the hospital?
The length of time you are in hospital depends on the extent of the surgery and how quickly you recover. On average, most people stay for seven to 10 days after the surgery.
Will I have pain?
You should expect some pain after your surgery. The surgical and anaesthetic team will make sure you have all the necessary pain relief prescribed on your drug chart so the nursing staff can provide it. If you are still in pain, please inform your doctor or nurse.
Will I have pain when I am home?
Each person’s pain threshold varies and so does the length of time each person has pain. Please, follow the guidelines below to manage your pain.
- Take your medications as directed and as needed.
- Call your doctor if the medication prescribed for you doesn’t relieve your pain.
- Do not drive or drink alcohol while you are taking prescription pain killers.
- As your wounds heal, you will have less pain and need less pain relief. Medications such as Paracetamol or Ibuprofen will relieve aches and discomfort in most individuals. Alternatively, stronger pain killers are prescribed, such as opioids (for example, Dihydrocodeine).
- Pain medication should help you as you resume your normal activities. Take enough medication to make sure you can gradually increase your activities. Pain medication is most effective 30 to 45 minutes after taking it.
- Keep track of when you take your pain medication. It will not be as effective if you allow your pain to increase. Taking it when your pain first begins is more effective than waiting for the pain to get worse.
- There is a number of different medications used to manage your pain, some of which are made from opium, which comes from the poppy plant, so called opioids or narcotics. These pain killers are generally safe when you take them on small doses for a short time, yet can potentially cause dependency if used for a long time or are misused. Follow your doctors guidance on receiving these medications if prescribed and report any feeling of dependency if applicable.
How can I prevent muscle wastage?
The ward physiotherapy will work with you to minimise muscle wastage while an inpatient and the outpatient physiotherapist will follow you after your discharge to work on your mobility and muscle power.
How can I prevent constipation?
Strong pain medication may cause constipation, but there are steps you can take to prevent it, including exercising if you can. Walking is an excellent form of exercise. Drink plenty of water and make sure you include plenty of fruit and vegetables in your diet. If these methods do not help, talk with your doctor or nurse. He or she may recommend over the counter or prescription medication
When will my stitches be removed?
We try to use absorbable stitches when we can, however, any non-absorbable stitches will be removed approximately two weeks after your surgery. The stitches may stay in place for longer if deemed necessary from your surgical team.
How do I look after my donor site?
It is quite important to keep donor site moisturised to improve its cosmetic appearance and avoid ugly scarring, soreness or itching. Details of aftercare and ointment application will be given to you from your surgeons upon discharge.
How do I care for my incisions?
- Do not apply direct heat or cold to the wounds. They may be numb, and you can easily burn yourself.
- Do not use hot water bottles or heating pads. You should also avoid saunas and steam rooms.
- Do not shave over your wounds while your stitches are in place
When can I shower?
Your surgeons will give you instructions on when you can shower.
When can I swim?
You can swim when you’ve been told that your wounds are completely healed. Avoid hot tubs, baths and swimming pools until then.
When can I resume my normal activities?
This depends on the extent of your surgery and how quickly you recover. On average 80% of patients get back to employment and can expect to get back roughly 75% of their limb function. It is important to realise that it can take a long time to get over an open fracture and that recovery can be on-going up to 18 months after the injury. The fracture may take over six months to heal. Doing exercises and physiotherapy play a key role once your orthopaedic surgeon is happy with the progress of your fracture healing.
When is it safe for me to drive?
You should only return to driving when you are able to perform an emergency stop. On average, this is about six weeks after you are able to fully bear your own weight, but this is different for each person, and their injury.
When can I exercise?
You may find that you may not be able to play sports as well as before, but able to manage with everyday functions. Do not do strenuous exercise or lift any objects heavier than 2kg for six weeks. Talk with your surgical team before resuming activities such as lifting and exercise.
When can I resume sexual activity?
Your doctor will tell you when you can resume sexual activity.
What type of follow-up care will I receive after I leave the hospital?
Both the Orthopaedic and Plastic Surgery teams will need to see you after discharge to monitor the healing of your fracture and soft tissue reconstruction. This is usually done in a joint clinic, (the Orthoplastics Clinic), and/or may be the Plastics Dressings Clinic (PDC). You will be informed of your follow up appointment date and time when you are discharged from hospital.
How can I cope with my feelings?
After surgery for a serious injury, you may have new and upsetting feelings. Many people say they felt weepy, sad, worried, nervous, irritable, or angry at one time or another. You may find that you cannot control some of these feelings. If this happens, it’s a good idea to seek emotional support.
The first step in coping is to talk about how you feel. Family and friends can help. Your nurse, doctor or physiotherapist can reassure, support, and guide you. It is always a good idea to let these professionals know how you, your family, and your friends are feeling emotionally. Many resources are available to patients and their families. Whether you are in the hospital or at home, your nurses and doctors are here to help you and your family and friends handle the emotional aspects of your illness.
What if I have other questions?
If you have any questions or concerns, please contact:
- The Orthopaedic or Plastic Surgery teams at the Royal Sussex County Hospital on 01273 696955
- Call the ward you stayed as inpatient via switchboard on 01273696955 to seek advice from the nursing staff. You can reach them Monday to Friday from 8am to 5.30pm
- Alternatively, email uhsussex.plasticsteam@nhs.net with any non-urgent queries.
Authors:
Dimitrios Kanakopoulos: Plastic & Reconstructive Trauma Fellow
Andrew Stone: SpR Trauma & Orthopaedics
Enis Guryel: Consultant Trauma & Orthopaedics/Major Trauma Lead
This information is intended for patients receiving care in Brighton & Hove or Haywards Heath.
The information in this leaflet is for guidance purposes only and is in no way intended to replace professional clinical advice by a qualified practitioner
Publication Date: June 2021
Review Date: March 2024


