Excision of urethral diverticulum
Download and print as a PDF
Download- What is a urethral diverticulum?
- Why do I need this kind of surgery?
- How did this happen?
- What can I expect before the operation?
- Will I have a general anaesthetic?
- What does the operation involve?
- What are the risks?
- What can I expect after the operation?
- What about going home?
- What about follow up?
- Who can I contact with any concerns or questions?
What is a urethral diverticulum?
Urethral diverticulum refers to out pouching of the wall of the urethra. This leads to a side pocket, where the urine accumulates. It can cause a swelling in the vagina, usually below the urethra.
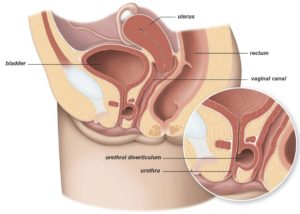
Urethral diverticulum
Why do I need this kind of surgery?
Urethral diverticulum can sometimes cause problems, such as perception of swelling, recurrent urinary tract infections or difficulty passing urine. It often leads to continued trickle of urine after you think you have completed passing urine.
How did this happen?
The out pouching of the inner wall of urethra happens as a result of a tear. Tearing at the time of vaginal delivery is the commonest cause. This tearing can be minute and undetectable at the time of delivery. However, it can become bigger with time, as the pouch becomes bigger with time.
What can I expect before the operation?
You will be invited for pre op assessment, when the nursing staff will go through your hospital stay and explain your operation. Please do let us know about any concerns you have or if there is any information you think we should know about that will make your stay with us more comfortable.
You will need to make arrangements for your family, children or any other commitments that you have, before coming in to hospital, and to cover the length of your recovery.
On admission, the nursing staff will go through your stay on the ward again to ensure you feel comfortable whilst in the hospital.
You will see an anaesthetist and the doctor performing the surgery before you go to theatre. It is not unusual to feel anxious; the nursing staff will gladly discuss how you are feeling and talk you through your emotions.
If you have not already signed the consent form when your operation was agreed and booked, the doctor will go through it with you before you go to theatre.
Will I have a general anaesthetic?
The operation can be done under general anaesthesia or spinal anaesthesia. The choice will depend on your preferences and other factors, such as whether you are breast feeding or not. Discussions about anaesthesia take place during clinic consultations, before booking.
What does the operation involve?
What does the operation involve?The operation is done through the vagina. The pouch is divided from the urethra and removed. The wall of the urethra is then closed with stitches. Sometimes, it is necessary to add another layer to support this closure. This may entail an additional incision parallel to the labia. A catheter will be inserted for few days, to help healing.
It is not uncommon to combine this with a camera examination of the inside of the urethra and bladder (cystoscopy). A separate information leaflet is available about this operation.
What are the risks?
There are risks with any operation but these are minor, as the operation is relatively minor. The main risks associated with this operation are:
Common risks:
- Postoperative pain. You will be provided with pain killers.
- Wound infection, which may need antibiotics.
- Wound bruising, breakdown and delayed wound healing.
- Difficulty passing urine. This is usually for a short period of time, to allow healing and resolution of any swelling caused by surgery. You may have a catheter for few days and then come to a clinic or the ward to have it removed.
Uncommon risks:
- Venous thrombosis and pulmonary embolism (blood clot in leg / lung). These are reduced by elastic stockings and injections that thin the blood to prevent clots.
- The urethral diverticulum may recur with time.
- Bleeding requiring blood transfusion.
- Return to theatre e.g. because of bleeding.
- Urinary fistula, where the site of the diverticulum does not seal and urine may pass through the residual home to the front passage. This can be dealt with by leaving the catheter for longer, to allow time for the area to heal. If healing does not happen, surgery might be required to close the area with sutures.
In order for you to make an informed choice about your surgery please ask one of the doctors or nurses if you have any questions about the operation before signing the consent form.
What can I expect after the operation?
As you come round from the anaesthetic you may experience episodes of pain and / or nausea. Please let the nursing staff know and they will assess you and take appropriate action.
You will have a drip to give you fluids, though you will be able to eat and drink. It is not unusual to experience lower back pain and a feeling of fullness in your bowel and generalised discomfort when sitting. We use a pain score to assess your pain 0 to 10: 0 No Pain, 10 Very Strong Pain.
Your nurse will be checking your blood pressure, pulse, respirations and temperature and monitoring any vaginal bleeding. S/he will also ask you to move from side to side and to do leg and breathing exercises once you are able, this will help prevent any pressure damage, a DVT (deep vein thrombosis) or chest infection.
What about going home?
The operation is usually carried out as a day case. You will be encouraged to sit up and start to walk, when you feel comfortable. You will be able to go home when you are passing urine without difficulty; unless you have a catheter, in which case you will be given a date to come back to have it removed
Please feel free to ask questions about your operation and recovery at any time. The nursing team will discuss your convalescence. To ensure you have a good recovery you should take note of the following:
Rest: During the first day or two at home, you might feel tired, exhausted and emotional. You should relax during the day, gradually increasing the number of things you do. You should be able to return back to normal within a week. Avoid crossing your legs when you are lying down.
Vaginal bleeding: You can expect to have some vaginal discharge / bleeding for few days after surgery. Sanitary towels should be used, and not tampons, to reduce the risk of infection.
Stitches: The wound in the urethra will be closed by dissolvable stitches and these do not need to be removed.
Housework: We recommend that you do light activities around the house in the first day or two days. You would expect to be back to normal within a week.
Showering: You will be able to have a shower shortly after the operation. However, it is better to avoid having a bath for 2 to 3 weeks, to ensure that the wound has healed.
Exercise: Exercise is important and it is advisable to go for short walks each day, increasing the distance gradually. You should avoid straining or heavy exercise for few days, to ensure good tissue healing.
You may return to normal exercise such as gentle cycling and swimming after 4 weeks. You will be able to manage the stairs on your arrival home. We encourage you to do pelvic floor exercises. You will be given a physiotherapy booklet titled ‘Fit for Life’ to guide you.
Diet: A well balanced nutritious diet with high fibre content is essential to avoid constipation. Your bowels may take some time to return to normal after your operation and you may need to take laxatives. You should include at least 5 portions of fruit and vegetables per day. You should aim to drink at least 2 litres of water per day.
Sex: You should usually be able to resume sexual activity within 4 weeks of the operation, to allow the vaginal wound to heal. If you experience vaginal dryness, you may wish to try a vaginal lubricant from your local pharmacy. If after this time you experience pain or any problems with intercourse then you should see your GP.
Returning to work: This will depend on the nature of your work. You can return back to work after a day or two. You may take a week off to avoid any discomfort from sitting down for a long time. A sick note can be provided, if required.
Driving: It is usually safe to drive within a week. However, this will depend on your level of concentration and ability to sit comfortably whilst driving. You may need to check with your doctor as well as your car insurance company.
What about follow up?
A follow up can be arranged, if required. This is usually organised for 12 weeks after surgery. If you have problems, you can either contact your doctor or contact the hospital to arrange for an appointment or bring an arranged appointment forwards.
Who can I contact with any concerns or questions?
You should contact your doctor or the hospital if you notice:
- Increased temperature.
- Wound swelling and / or pain.
- Smelling discharge either from the wound or the vagina.
- Blood in urine or stools (poo), abdominal distension and / or failure to open your bowel.
If you have any problems or questions, you can contact:
The Urogynaecology Unit at Lewes Victoria Hospital on 01273 474 153 Extension 2178 (from 09:00 till 17:00 Monday to Friday).
The Gynaecology Ward at the Princess Royal Hospital on 01444 441 881 Extension 5686.
The Gynaecology Ward at the Royal Sussex County Hospital on 01273 696 955 Extension 4013.
References / useful links:
British Association of Urological Surgeons: Removal of the diverticulum from the urethra
If you do not understand this leaflet, we can arrange for an interpreter.
This information leaflet has been produced by Dr. Sharif Ismail, Consultant Subspecialist Urogynaecologist.
This information leaflet has been approved at the Clinical Governance and Safety and Quality Meetings of the Department of Obstetrics and Gynaecology as well as Brighton and Sussex University Hospitals.
This information is intended for patients receiving care in Brighton & Hove or Haywards Heath.
The information in this leaflet is for guidance purposes only and is in no way intended to replace professional clinical advice by a qualified practitioner.
Publication Date: March 2021
Review Date: December 2023


