Bronchiectasis
Download and print as a PDF
Download- What is bronchiectasis?
- What causes bronchiectasis and how did I get it?
- What are the symptoms and why do I have them?
- How is bronchiectasis diagnosed?
- How do I recognise an infection?
- How is bronchiectasis treated?
- How can I manage my bronchiectasis?
- Active Cycle of Breathing Technique (ACBT)
- Contact details if you need further information or advice
What is bronchiectasis?
Bronchiectasis
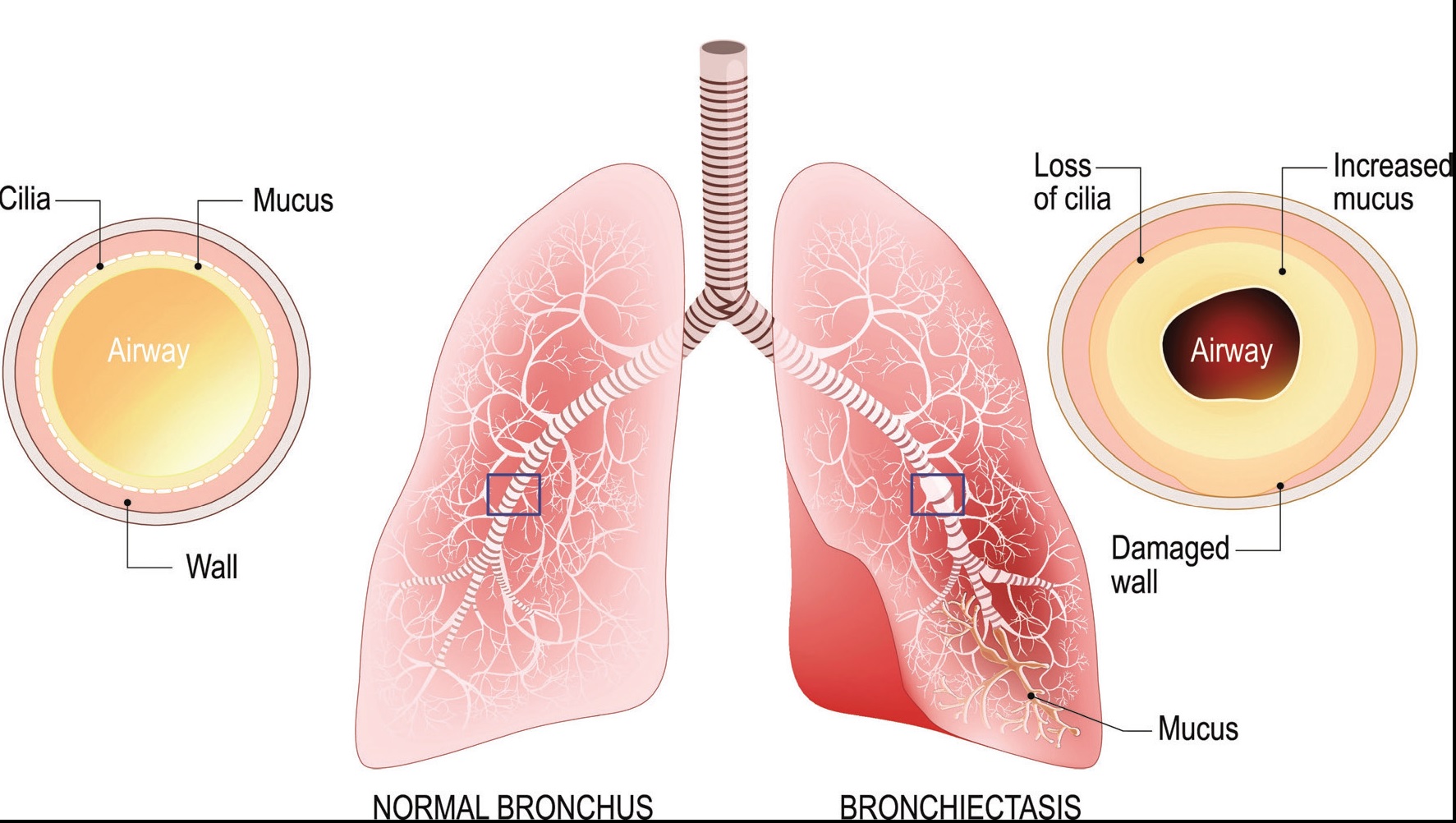
Bronchiectasis is a condition where the airway (bronchi) in the lungs become widened and damaged.
In healthy lungs a small amount of mucus is secreted into the bronchi. This acts as a protective lining, trapping dust and bacteria that have been breathed in. To prevent a build-up of this mucus, the bronchi are lined with microscopic hairs, called cilia, which clear the mucus from the airways.
In bronchiectatic lungs these cilia do not effectively clear the mucus so it builds up, making the bronchi prone to infections which can spread. If you get repeated infections, the bronchi can become permanently widened and damaged. This damage results in permanent lung inflammation, and overproduction of mucus from the mucus glands.
To find out more about bronchiectasis, have a look on the British Lung Foundation website.
What causes bronchiectasis and how did I get it?
There is often no obvious cause, but it may be because of one or more of the following:
- Mechanical causes, for example, inhalation (breathing in) of a foreign body.
- Damage to the lung from previous (often childhood) illness. TB, measles, whooping cough and pneumonia can all result in scarring of the lungs and a reduced immunity to further lung infections.
- Immunodeficiency syndromes, for example, HIV.
- Poor cilia action, for example, ciliary dyskinesia. There is where the cilia do not move at the same time, so it is more difficult to clear the mucus from the airways.
What are the symptoms and why do I have them?
The symptoms of bronchiectasis can include:
- A cough, producing mucus or phlegm. This is because of an increase in the amount of mucus produced in the lungs and/or poor mucus clearance.
- Wheeze. This is because of a narrowing of the airways caused by muscle spasm.
- Shortness of breath. This happens as a result of inflammation, which reduces the elasticity and muscle tone in the bronchial tubes. These then collapse and become infected.
- Other symptoms can also include: runny nose or chronic sinusitis, coughing up blood (haemoptysis), chest and joint pain
How is bronchiectasis diagnosed?
Bronchiectasis is diagnosed by:
- Chest x-ray
- CT scan
- Bronchoscopy
- A bacterial check, called sputum culture
- Lung function tests. These show the volume of air you are capable of breathing out, and how forcefully you can breathe out.
- Blood tests (white blood cell count), to find out whether there is any active infection.
How do I recognise an infection?
You may have one or more of these symptoms if you have an infection:
- An increased amount of sputum.
- Green, yellow, grey or brown sputum.
- Increased frequency and duration of cough, including night coughing.
- Blood stained sputum. This is caused when small blood vessels in the lungs become damaged, usually because of excessive coughing.
- Increased breathlessness and a reduced exercise tolerance.
- Change in taste or smell of your sputum. If you notice any or all of the above symptoms, you should see your GP as soon as possible.
How is bronchiectasis treated?
In the 1950 and 1960s lung surgery for bronchiectasis was quite common. Nowadays, surgery will only be performed if a patient has severe but localised disease.
In the case of a severe exacerbation or a ‘flare-up’, it may be necessary to admit you to hospital where more intensive treatment can be given.
Here are some common medications to treat bronchiectasis. Your doctor will decide which is most appropriate for you:
Steroids These reduce inflammation and the amount of sputum produced.
Antibiotics This is to treat infection.
Bronchodilators This makes breathing easier and reduces breathlessness and wheezing by reducing muscle spasm in the bronchi. For more information about treatment for bronchiectasis, have a look at the British Lung Foundation website.
How can I manage my bronchiectasis?
- Give up smoking and avoid exposure to passive smoke. Ask your healthcare provider for techniques to help you give up smoking.
- Get a flu vaccine every year in the autumn and a one-off pneumococcal vaccine from your GP.
- Exercise regularly. This helps you breathe more easily by improving your muscle strength and tone and helps improve mucus clearance from the airways. Ask your physiotherapist about this if you have any questions.
- Eat a well-balanced diet and drink plenty of fluids. Minimise caffeinated drinks.
Active Cycle of Breathing Technique (ACBT)
This improves breathing control and helps to remove secretions. It should ideally be completed until the huff has been dry with no sputum on two consecutive cycles, although some patients will always have some residual sputum.
This can be done in sitting or
It has three parts:
1. Breathing control: this is gentle breathing at your normal rate, with your chest and shoulders relaxed.
2. Deep breathing: these are deep breaths which are each held for a few seconds. This assists the air flow behind the secretions which makes it easier for you to remove them. If done correctly, your stomach should gently rise as you breathe in.
3. Huffing: this helps move secretions from the lungs into the mouth. It is more effective than coughing and should not cause wheezing. The air is breathed out through contraction of the stomach muscles. It is a similar technique to misting up a mirror.
The physiotherapist will show you how to complete the ACBT. The more you practise it, the easier and more effective it will become.
Other information:
- Positioning. Gravity can be used to assist the clearance of secretions. Your physiotherapist will show you specific lying positions. Each position must be maintained for a minimum of 10 minutes in order to be effective. The ACBT can also be done in these positions.
- You may be given other equipment to help remove secretions including Acapella. Your physiotherapist will assess the need for this and teach you how to use it.
- Breathing control during activity. This can reduce breathlessness during activities e.g. climbing stairs, walking, and has been described in the Active Cycle of Breathing Technique section.Breathing control can be combined with postures to reduce breathlessness, including relaxed sitting, forward-lean standing, relaxed standing and forward-lean sitting.
For more information about physiotherapy exercises, have a look at the Association of Chartered Physiotherapists in Respiratory Care website.
Contact details if you need further information or advice
If you have any more questions about this booklet or need further information, please contact your physiotherapist.
Princess Royal Hospital: 01444 441881, ask for bleep 6224.
Royal Sussex County Hospital: 01273 696955, ask for bleep 8498.
Please contact us if you need this leaflet in an alternative language.
This information is intended for patients receiving care in Brighton & Hove or Haywards Heath.
The information here is for guidance purposes only and is in no way intended to replace professional clinical advice by a qualified practitioner.
Publication Date: May 2021
Review Date: February 2024


