Gallstones advice for patients seen in the Emergency Department
Download and print as a PDF
DownloadWhat are gallstones?
Your gall bladder is a small sac that lies beneath your liver, below the right rib cage. It stores and concentrates bile, a greenish-brown liquid formed by your liver. The bile then passes into your small intestine through bile ducts, to help with digestion, mainly of fats.
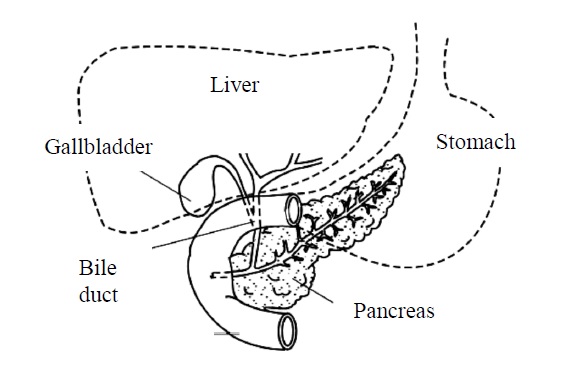
Location of the gallbladder
Gallstones are collections of crystals of various substances in the bile, especially cholesterol. They grow in the gall bladder and look like small stones.
Around 5.5 million adults in the United Kingdom have gallstones. They are more common in women than men, but overweight people and those over 60 seem to be more at risk. Gallstones may stay in the gall bladder or move into the bile duct (the tube between your liver and intestine).
There are a number of treatment options, if the gallstones are causing symptoms, including medicines, surgery, removal via an endoscope or using shockwaves.
The symptoms of gallstones
Not all gallstones cause symptoms. Often, people do not know that they have them. However, common symptoms of gallstones include
- Upper abdominal pain, which can be central or towards the right side of your body. It can be severe, intermittent, and last for hours. It may be hard to find a comfortable position to sit or lie down in.
- Longer lasting pain under the rib cage on the right-hand side, with tenderness or pain when you move.
- Nausea/bloating.
All the above symptoms may be triggered by a fatty meal.
If the gallstones move from your gall bladder into your bile duct, you may also experience
- Jaundice. Yellowing of your skin or eyes, sometimes with dark urine or pale motions (stool). This may happen if the bile duct becomes blocked with gallstones.
- Upper abdominal pain from inflammation (swelling) of your pancreas, known as pancreatitis.
- Fever caused by an infection from inflammation of the bile ducts (cholangitis) or the gall bladder (cholecystitis).
Tests for gallstones
Once gallstones are suspected, tests are likely to be performed to confirm their presence and location. These include
- An abdominal ultrasound scan. This is very similar to a pregnancy scan.. Ultrasound scans can identify the presence of gallstones, particularly in the gall bladder.
- Blood tests. These may give information about the causes of your gallstones and whether they may have moved to the bile duct.
- Endoscopic procedures. An instrument with a tiny camera or ultrasound on the end (called an endoscope) can be inserted through your mouth into the first part of the intestine to confirm the presence of stones in your bile duct.
- Additional scans. In some cases, scans such as Magnetic Resonance Imaging (MRI) or Computerised Tomography (CT) scans may be helpful in diagnosing gallstones.
Living with gallstones
Gallstones grow in the gall bladder and can cause episodes of pain, especially after fatty foods or a large meal. The pain is often cramping and intermittent but usually goes away after a few hours.
Reducing the size of your meals and eating a well-balanced diet may reduce your symptoms whilst you are waiting to have treatment.
If you find any particular foods trigger your symptoms, you could trial avoiding them to see if this helps.
Some people find that following a low fat diet can prevent episodes of pain from gallstones, or make them less frequent. However, this is not necessarily the case for everyone.
If you are overweight, gradual weight loss can reduce the risk of developing gallstones.
If you have persisting pain, fever or jaundice (yellowing of your skin or eyes), please seek prompt medical attention.
Further support
- For general medical advice please use the NHS website, the NHS 111 service, walk-in-centres, or your GP.
- NHS website provides online health information and guidance www.nhs.uk
- There are walk-in and urgent treatment services at Brighton Station, Crawley Urgent Treatment Centre, Lewes Victoria Hospital, Horsham Minor Injuries Unit and Bognor Regis War Memorial Hospital.
The information in this article is for guidance purposes only and is in no way intended to replace professional clinical advice by a qualified practitioner.
Publication Date: July 2022
Review Date: April 2025


