Acute interventional treatment for stroke (thrombectomy)
Download and print as a PDF
DownloadWhat is happening?
The doctors and nurses looking after you think that your symptoms may be caused by a blood clot blocking blood supply to the brain.
If left untreated this may result in a disabling stroke. A stroke can potentially cause limb weakness,
speech difficulty, visual changes and other complications. Quick treatment is needed to restore the blood supply to the affected area of the brain.
How can this be treated?
The first line of treatment is a drug called Alteplase. This is a clot-busting drug. The administration of this drug is known as 'thrombolysis'. The aim of thrombolysis is to dissolve the clot and get the blood flowing back to the affected area of the brain.
Thrombolysis must be given within 4.5 hours from the start of symptoms to stand a good chance of being effective.
In some people, Alteplase cannot be given if there are significant bleeding risks.
Some people may be suitable for an additional procedure to remove the clot mechanically. This is called a thrombectomy.
How is a thrombectomy performed?
A thrombectomy involves a thin plastic tube (catheter) being inserted, usually through an artery in the groin.
The catheter is then moved, through the blood vessels in your body, to the blocked blood vessel in your brain.
A contrast agent (dye) is injected into the catheter and X-ray is used to guide the catheter to the affected blood vessel safely.
A clot‑ retrieval device is moved through the catheter to the site of the blockage to remove the clot and re‑establish blood flow to the affected part of the brain.
A doctor called an interventional neuro radiologist will perform the thrombectomy. A radiographer will operate the X-ray equipment. Nurses will be available to assist during the procedure and to monitor and reassure you.
Most procedures are performed awake using local anaesthetic to numb the groin.
Sedation may be used if you become restless. Being restless is usually symptomatic of a stroke. Sedation helps to reduce the risks to restless patients.
In some cases an emergency general anaesthetic may be required. The procedure may be abandoned if it becomes too unsafe due to you being too unwell or too restless to tolerate it.
Occasionally, it may not be technically possible to retrieve the clot. This can be due to damaged or blocked blood vessels.

The neuro-angiography suite at the Royal Sussex County Hospital, Level 5, Millennium Wing
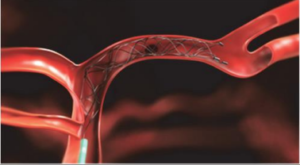
A stent retrieval device used to remove a clot in a brain vessel.
What are the benefits of thrombectomy?
Removing the blood clot from the blocked vessel leads to better outcomes including greater independence and mobility. Not every patient will benefit (because some damage to the brain has already happened) but 8 out of every 20 patients that undergo thrombectomy will recover with less disability. Severe complications from the procedure happen infrequently (in less than 1 in 20 patients) and the chances of a bad outcome do not increase as a result of this procedure.
What are the risks of thrombectomy?
The risks include:
- The contrast agent.
(the ‘dye’ we use to see the arteries and veins on X‑ray pictures). This carries a small risk of an allergic reaction. In rare cases, it can permanently harm the function of the kidneys. - Bruising/bleeding.
This sometimes occurs around the groin where the catheter is inserted. Only in very rare cases is this severe enough to require surgery to repair the groin artery. Problems that are rare but more
serious can include:- Worsening of the stroke (limb weakness, speech difficulty, visual changes and coma)
- Perforation of an artery leading to a bleed in the brain (potentially fatal).
Before we can go ahead with treatment, by law we must explain the risks and benefits to you, discuss alternative treatment options, and then seek your consent.
If you are too unwell to be able to give informed consent, the doctors will proceed in your best interests,
but will make every effort to involve your relatives in the discussion of consent. This discussion will include your known wishes and beliefs, and whether treatment is likely to be in your best interests.
What to expect after the thrombectomy
After the thrombetomy procedure has finished you will be taken to the stroke ward and cared for there by the stroke team and physicians.
You will be on bed rest for a couple of hours to allow the puncture site to heal, as well as your vital observations being checked regularly.
You can expect to experience some pain from the groin. This can be managed on the ward with analgesia.
Useful information
Stroke Association
www.stroke.org.uk
Helpline – 0303 3033 100
This website enables you to find stroke support groups and information in your local area.
The stroke wards at The Royal Sussex County are Donald Hall ward and Solomon ward. They are located on the third floor of the Barry Building.
The main contact for the stroke ward is Mark Holmes - 01273 696955 ext.4006
This information is intended for patients receiving care in Brighton & Hove or Haywards Heath.
The information in this leaflet is for guidance purposes only and is in no way intended to replace professional clinical advice by a qualified practitioner.
Publication Date: December 2019
Review Date: January 2023


