Botulinum toxin A: bladder wall injection
Download and print as a PDF
Download- What is botulinum toxin 'A'?
- Why do I need such an injection?
- What can I expect before the operation?
- What does the operation involve?
- What are the risks?
- What can I expect after the operation?
- What about going home?
- What about follow up?
- Are there any alternatives to botulinum toxin 'A' bladder wall injection?
- Who can I contact with any concerns or questions?
What is botulinum toxin 'A'?
Botulinum toxin is a chemical that relaxes muscles. It is commonly used for wrinkles on the face. In the bladder, it relaxes the bladder muscle, so as to reduce the urge to go to the toilet. There are two types, ‘A’ and ‘B’. Type ‘A’ is used in clinical practice, as it has a longer duration of action than type B.
Why do I need such an injection?
Botulinum toxin ‘A’ bladder wall injection is given to patients who suffer from overactive bladder that does not respond to at least two different types of medication.
Overactive bladder is associated with increased sensation from small volumes of urine in the bladder, with or without making the bladder contract (go into spasm).
As a result, patients feel they need to go to the toilet and may actually leak if they are not quick enough. Consequently, they go to the toilet a lot and may reduce their activity for fear of leakage.
What can I expect before the operation?
At your pre op assessment and on your admission day the nurse will go through your hospital stay and explain your operation. Please do let us know about any concerns you have or if there is any information you think we should know about that will make your stay with us more comfortable.
You will need to make arrangements for your family, children or any other commitments that you have prior to coming in to hospital and to cover the length of your recovery.
On the day, you will see the doctor performing the operation, who will be able to answer any questions. If you are having the operation under anaesthesia, you will also see an anaesthetist, who will answer any questions about anaesthesia.
If you have not already completed a quality of life questionnaire, you might be asked to do so before surgery. Likewise, if you have not already signed the consent form on booking, the doctor will go through it with you before you go to theatre.
You will be asked for permission to enter your data on the national database for continence and prolapse surgery. This is a quality control measure to compare the safety and effectiveness of such procedures at the hospital against other units in the country.
You will be given a frequency volume chart and quality of life questionnaires to complete and bring with you as you attend for follow up after surgery. This will enable assessing the benefit of surgery for you.
What does the operation involve?
Injections are given using a telescope (camera) passed through the urethra (cystoscopy). This can be done under general or local anesthesia. This is usually as a day case and you will be able to go home on the same day.
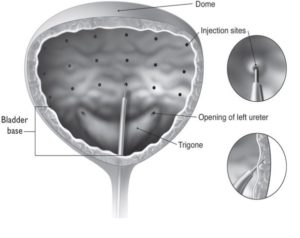
Botulinum Toxin A: bladder wall injection
What are the risks?
There are risks with any operation but these are small. The main risks associated with botulinum toxin ‘A’ bladder wall injection are:
Common risks:
- Blood stained urine. This is to be expected and should settle on its own within few days.
- The most frequent problem is initial difficulty in passing urine. This happens as a result of over relaxation of the bladder muscle. Patients may need to pass a catheter to help emptying their bladder themselves; a practice called intermittent self catheterisation. It is therefore important that patients are aware of this possibility and able to perform clean self catheterisation themselves, in case they have to do this after the injection.
- Recurrence of overactive bladder symptoms. This may happen between 6 to18 months. It may necessitate a repeat injection, which is usually carried out every year or two years.
- Postoperative pain, which is usually mild and lasts for a day or two.
- Urinary tract infection, which may need antibiotics.
Uncommon risks:
- Venous thrombosis and pulmonary embolism (blood clot in leg / lung). These are extremely rare after such a minor operation.
- Failure to improve or cure overactive bladder symptoms. This is rare and may require alternative treatment.
- Allergic reactions can happen, but they are extremely rare. These take the form of general malaise and possible rash. You will need to contact your doctor or the hospital for medication.
In order for you to make an informed choice about your surgery please ask one of the doctors or nurses if you have any questions about the operation before signing the consent form.
What can I expect after the operation?
Immediately after the operation, you may experience episodes of pain and / or nausea. Please let the nursing staff know and they will assess you and take appropriate action.
You will be able to go home when you are passing urine without difficulty. You will be asked to pass urine in a jug and will have a scan to measure how much urine is left in the bladder. It helps to forget that you need to pass urine and drink and walk as you would normally do, and this is when your bladder is likely to work as normal.
If your bladder does not empty properly, it will be emptied with a catheter. You might be shown how to do clean intermittent self catheterisation.
What about going home?
Most patients go home on the same day. The nursing team will discuss your convalescence. To ensure you have a good recovery you should take note of the following:
Rest: During the first few days at home it is common to feel tired, exhausted and emotional. You should relax during the day and gradually increase the number of things you do each day. Avoid crossing your legs when you are lying down.
Blood stained urine: This should settle within few days.
Incomplete bladder emptying: After going home, you will be asked to keep an eye on passing urine. If you feel your bladder is holding back some of the urine, you can ring your doctor or the hospital to come for a bladder scan.
Housework: You should be able to resume normal daily activities within few days.
Exercise: Exercise is important and it is advisable to go for short walks each day, increasing the distance gradually. We encourage you to do pelvic floor exercises. You will be given a physiotherapy booklet titled ‘Fit for Life’ to guide you.
Diet: A well balanced nutritious diet with high fibre content is essential to avoid constipation. Your bowels may take some time to return to normal after your operation and you may need to take laxatives. You should include at least 5 portions of fruit and vegetables per day. You should aim to drink at least 2 litres of water per day.
Sex: You should usually be able to resume sex within 1 to 2 weeks after the operation. There is no vaginal wound. It all depends on whether you feel any pain or not and how you are passing urine.
Returning to work: You should be able to return to work within a week. You can provide a self certificate or the hospital doctor will provide you with one.
Driving: It is usually safe to drive within a week. This will depend on your level of concentration and ability to perform an emergency stop. Please check with your insurance company.
What about follow up?
You will be invited for follow up, usually about 12 weeks after surgery. If you have problems before this you can either contact your doctor or contact the hospital to bring the appointment forwards.
During this follow up appointment, your symptoms will be reviewed. The frequency volume chart and quality of life questionnaire will be checked.
Are there any alternatives to botulinum toxin 'A' bladder wall injection?
Alternative procedures for overactive bladder include:
Percutaneous tibial nerve stimulation: This entails stimulation of a nerve behind the ankle. This nerve shares the same root with the bladder nerve supply. Its stimulation leads to reduction of bladder contractions and therefore overactive bladder symptoms. There is no risk of incomplete emptying of urine, and therefore there is no need for intermittent self catheterisation. However, attendance is required for 12 weekly sessions, which may not be convenient for some patients. This requires funding approval for individual patients at the moment.
Sacral neuromodulation: This technique entails direct stimulation of the centers that control the nerve supply to the bladder in the spinal cord. This is a bigger procedure that requires anaesthesia.
It is carried out in two stages. It requires the insertion of needles between the bones of the vertebral column. The operation has potential for more complications. This requires funding approval for individual patients at the moment.
Bladder wall surgery: This entails expanding the bladder using bowel segment. The hope is to reduce the effect of bladder muscle contractions. This operation is rarely performed nowadays.
Diversion of urine to the bowel: It is seldom performed nowadays and is always a last resort.
These can be discussed with your doctor.
Who can I contact with any concerns or questions?
You should contact your doctor or the hospital if you notice increased temperature, frequent need to pass urine, which might be smelling or hurting.
If you have any problems or questions, use the contact numbers below to contact us.
Princess Royal Hospital: 01444 441881 extension 5686
Royal Sussex County Hospital: 01273 696955 extension 4013
Urogynaecology Unit at Lewes Victoria Hospital: 01273 474153 extension 2178
Further source of information:
This patient information leaflet was prepared by Dr. Sharif Ismail, Consultant Subspecialist Urogynaecologist.
This information leaflet has been approved at the Clinical Governance and Safety and Quality Meetings of the Department of Obstetrics and Gynaecology as well as Brighton and Sussex University Hospitals NHS Trust Carer and Patient Information Group (CPIG).
Ratified April 2017 Women’s Safety and Quality Committee.
This information is intended for patients receiving care in Brighton & Hove or Haywards Heath.
Disclaimer
The information in this leaflet is for guidance purposes only and is in no way intended to replace professional clinical advice by a qualified practitioner.
Publication Date: May 2021
Review Date: February 2024


