external cephalic version
Download and print as a PDF
Download- What is an External Cephalic Version (ECV)
- Why do I need an ECV and what are the benefits of having one?
- When is ECV done?
- Are there any risks to my baby if I choose to have ECV?
- Are there any alternatives to ECV ?
- What will happen if I decide to have ECV?
- What if my blood group is Rhesus Negative?
- References
What is an External Cephalic Version (ECV)
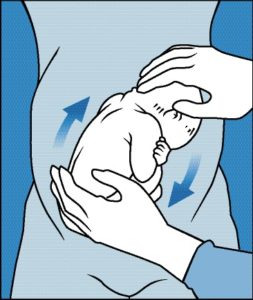
An ECV involves a clinician trying to turn your baby from a bottom down position into a head down position. This is done by giving you an injection to relax your womb. Once this is effective the clinician will try to turn your baby by using their hands to feel the baby through your tummy and pushing the baby round into the head down position. The method has a 50% success rate of achieving moving baby to a head down position.
External cephalic version
Why do I need an ECV and what are the benefits of having one?
You will be offered an ECV when your baby is lying bottom down in your womb (called breech position). Some babies who are in a breech position may be at more risk during birth than those who are born head first (cephalic position). For this reason we offer you the option of trying an ECV.
If ECV is not possible or does not work, you will be offered the choice of a caesarean delivery or a vaginal breech birth. Please see the parent information leaflet on ‘Breech’ for more detail about your birth options (available on our website: www.mypregnancymatters.org.uk). Your midwife or doctor will be happy to discuss this further with you and will support you in making the decision that is right for you.
When is ECV done?
You will be offered an ECV from 36 weeks onwards but it can be undertaken at any time up to when you go into labour.
Are there any risks to my baby if I choose to have ECV?
Generally ECV is very safe. Occasionally we will hear changes in the baby’s heart rate during or after the procedure. In most cases, babies recover quickly and are not adversely affected. In a very small number of cases (5 in 1000) the heart rate may show the baby is becoming distressed and we may need to deliver the baby by caesarean section.
Sometimes, if your baby is small or the amount of fluid around the baby is reduced then we may advise against ECV. Also, if you have had a previous caesarean section, we may suggest this is not appropriate, but your obstetrician can advise you on an individual basis.
Are there any alternatives to ECV ?
There is a type of heat therapy called moxibustion (Chinese medicine which involves burning a herb close to the acupuncture point located at the tip of the fifth toe) which may help turn babies from breech to the head down position. Acupuncture may also be of benefit. We advise that you go to an appropriately qualified practitioner for these procedures as we do not currently offer them here in the Trust.
You may also want to try optimal fetal positioning, where you maximise the space in your pelvis and encourage the baby to move round by adopting different positions, for example rocking on all fours. Although research studies do not yet show us that this may help turn the baby to be head down, it may be of benefit to help the baby get into a good position.
What will happen if I decide to have ECV?
You will be asked to come to the labour ward RSCH (Level 13) or the labour ward PRH. Please do not eat anything from 8.00am until after the ECV. We advise you drink water. This is due to the very small risk that you may need a caesarean section. When you arrive you will be seen by a midwife who will check you and your baby’s wellbeing. The obstetrician will perform a scan to check that the baby is still in a breech position and afterwards the baby’s heart rate will be checked. You will then be given an injection which helps to relax the womb and makes the ECV more likely to work. The drug used is called terbutaline and the injection is given into the arm, just under the skin (subcutaneously). 20 – 25 minutes after the injection the obstetrician will attempt to turn the baby. The ECV can be uncomfortable, because of the pressure on your tummy, but should not be painful.
After the ECV, whether it is successful or not, the baby will be monitored again using a cardiotocograph (CTG) for about 20 – 30 minutes. If the ECV is successful you will continue with the usual care by your midwife. There is a small chance that the baby will naturally turn back to breech again. Your midwife will check your baby’s position at every appointment and advise you if this occurs.
If the ECV is unsuccessful we will discuss your options. A few women can have a second attempt at ECV; your obstetrician will advise if this is appropriate for you at the time. We will provide you with further information about your options for the birth of your baby. Further information and a leaflet about breech presenting babies are available on our website www.mypregnancymatters.org.uk. Remember, some babies will spontaneously turn from breech to head down themselves in the last few weeks, so we will re-check the baby’s position when we see you or before any planned birth.
What if my blood group is Rhesus Negative?
If you have a Rhesus negative blood group you should have already been offered an Anti-D injection during your pregnancy and be aware of why this is needed. During the ECV it is possible for the baby’s cells to mix with yours and it is recommended that you have an extra Anti-D injection following the ECV, whether it was successful or not, to deal with these cells.
References
1. Royal College of Obstetricians and Gynaecologists. Guideline No. 20b THE MANAGEMENT OF BREECH PRESENTATION December 2006.
2. Royal College of Obstetricians and Gynaecologists. Guideline No. 20a External Cephalic Version And Reducing The Incidence Of Breech Presentation. December 2006.
This information is for guidance purposes only and is in no way intended to replace professional clinical advice by a qualified practitioner.
This article is intended for patients receiving care in Brighton & Hove or Haywards Heath.
Publication Date: August 2016
Review Date: January 2023


