breastfeeding in the first few days
Download and print as a PDF
DownloadWhat this information is about
Establishing breast feeding can be really challenging. Your baby may want to feed very frequently and this can feel really hard especially when you are very tired, during the night and if your nipples are sore. We are here to help support you during this time to establish breastfeeding, both on the post natal wards and at home. This leaflet offers some useful tips and practical advice about breastfeeding in the first few days that we hope you will find useful.
Frequency of Feeding
Babies vary in the frequency of their feeding in the first 48 hours. Many feed frequently for short periods, whilst others may not feed very much in the first 24 hours and then want to feed a lot. A baby’s stomach at birth is tiny (about the size of a hazelnut) and it does not need much to fill it. Even though you may think that you are producing only small amounts it matches the size of the baby’s stomach.
Night feeds
Night time feeds are particularly valuable because the milk-producing hormone Prolactin is present in larger quantities at night. So night feeds are really important for building up your milk supply. Surprisingly, night feeds also have a relaxing effect; the quality of sleep improves due to the breastfeeding hormones produced. It has been proven that women who breastfeed have a better quality of sleep and get back to sleep quicker than mothers who bottle feed. If it is your first baby, and the baby has fed a lot at night, have a lie in the following morning.
Sore nipples
Sore nipples are caused by the baby being incorrectly attached to the breast, rather than suckling itself. When positioning and latch are corrected, feeding will immediately become more comfortable, and even very tender nipples will heal quickly.
Reading your baby
Babies have many ways of letting you know they need food. They only begin to cry to be fed once the other signals they have given have not been recognised. Some newborn babies will not have the energy to cry and may just go back to sleep if the feeding cues are not responded to.
Infant feeding cues
- Rapid eye movements seen under closed eyelids.
- Flexing of arms while still asleep.
- Making sighing noises.
- Lip sucking.
- Mouth gaping.
- Rooting and putting hand to mouth.
- Following their hand with gaping mouth.
- Waking and making quiet eye contact.
This sequence of non-verbal cues lasts for approximately fifteen minutes. If the above body language is not responded to, most babies will cry. Some, however, will simply go back to sleep to conserve energy.
It is recommended that you respond to the early cues. Babies that are learning to breastfeed, often feed better when they are coming out of a sleep, rather than very hungry and upset. This is called responsive feeding and allows for babies to find comfort as well as food at the breast.
We now know that keeping our babies close and responding to their cues for food, comfort and love is important for their brain growth and this closeness helps to foster close family relationships, which are good for long term health and wellbeing.
How an artificial feed may affect breastfeeding.
- Breastfeeding works on a supply or demand basis. The more the baby feeds the more milk is produced. If a baby is given an artificial feed it will take longer to digest and she or he will not want to suckle for some time. This affects this natural balance of supply or demand and thus less milk is produced.
- If the baby does not breastfeed often enough, your breasts may become full. This can be painful and may make it difficult for the baby to attach correctly.
- Artificial feeds alter the bacteria in the baby’s gut. This may increase the risk of your baby developing infections.
- Artificial feeds may potentially increase the risk of asthma, diabetes obesity and allergies, particularly if there is a family history.
- A baby uses the tongue, jaws and mouth differently when sucking on a bottle. If a baby is given a bottle at this early stage, she/he may find it more difficult to learn to suckle at the breast as a very different technique is practised when bottle feeding.
Breast milk: how much does my baby need?
Your baby’s tummy is tiny at birth, with a stomach capacity of around 5 to 7 millilitres. It is about the size of a hazelnut. This increases over the first few days to 22 to 27 millilitres at 3 to 5 days. By 10 to 12 days the capacity expands to 60 to 85 millilitres (about the size of a walnut!).
Don’t worry about your milk production, providing that the baby is feeding regularly at the breast or you are expressing 8 to 12 times a day our milk supply will increase to match your baby’s growing appetite.
Count the number of wet nappies: baby should be producing at least two on day two, three on day three, four on day four and at least six wet nappies a day thereafter. The volume of urine in the nappy should increase along with the increase in number of wet nappies. Note the colour of dirty nappies. The stool should be changing from the sticky, dark meconium by day three, be brown by day four and become a yellow colour by the fifth day.
If your baby does not have a dirty nappy for more than 24 hours or the stools are not changing colour in the first five days, you should seek advice from a midwife.
The following is a guide for mothers who need to express milk for their babies.
Breastmilk: Average volume produced
| Age. | Amount per day. |
Amount per feed. |
Wet nappies/ day. |
| Day 1 | 37 mls | 2 - 7 mls | |
| Day 2 | 84 mls | 14 mls | 2 - 3 |
| Day 3 | 408 mls | 38 mls | 3 - 4 |
| Day 4 | 625 mls | 58 mls | 4 - 5 |
| Day 5 | 700 mls | 70 mls | 6 + |
| 3 months | 750 mls | 6 + | |
| 6 months | 800 mls | 6 + |
Hand expressing
You can practice the technique toward the end of your pregnancy from 36 weeks, so that you feel comfortable with it. Start again as soon as possible after your baby is born, while you are on labour ward, during skin to skin. This may stimulate your baby to feed and if not, provide valuable colostrum, you can express onto babies lips. Every drop is precious.
Hand expressing is really useful when you have a sleepy baby who needs colostrum in the first 24 to 48 hours, but is not able to feed.
It is also helpful when your baby has been admitted to Special Care at the PRH or the Neonatal Unit at the RSCH. By hand expressing you can stimulate your milk supply and your colostrum will be given to your baby. When the baby is well enough to breastfeed you will have a ready supply. It is recommended that you start hand expressing within 6 hours of the birth.

What do you do?
Hair brushing and shoulder massage before and during your expressing will relax you and increase Oxytocin levels. Massage your breasts for a few minutes. Use flat of fingers, and gently move around the breast, gradually work your way towards the nipple and areola. Do not drag your fingers over your skin. About five minutes of massage will help the milk to flow. Some women make a fist and gently knead the breast, do not drag the skin, move around the breast in circular movements, gradually working down to the areola. Rolling your nipple between your finger and thumb stimulates Prolactin output.
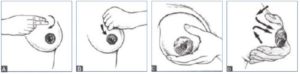
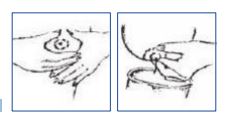
When you are ready to start expressing, place your thumb on top of your breast approximately 2cms away from the base of the nipple, place your index finger the same distance away from the base of the nipple, underneath your breast.
Push back into breast tissue a little, and then gently compress the breast. You can move finger and thumb, around the breast so that you express all areas. Ask a member of staff to talk you through it.
Do not be concerned if you do not see anything at first, just keep trying and it will come. To establish your milk supply, if baby is not feeding in the first 24-48 hours try to hand express for about 100 minutes in 24 hours. This sounds a lot, but if you hand express for five minutes every hour, you will be doing fine, and if you were able to do more, so much the better. The trick is not to be put off if you do not see anything at first, the repeated hand expression will trigger the production of colostrum as the day goes on, and in the course of a day you can go from nothing, to a few beads by lunchtime to collecting colostrum into a syringe for baby by late afternoon! Babies only need small amounts of colostrum in the first day and even tiny beads of colostrum are packed with components which reduce risk of infection; increase baby’s ability to use alternative energy stores in the first two days, and help protect against future illness.
Contact details
This information is for guidance purposes only and is in no way intended to replace professional clinical advice by a qualified practitioner.
This article is intended for patients receiving care in Brighton & Hove or Haywards Heath.
Publication Date: December 2019
Review Date: November 2022


