Hysteroscopy
Download and print as a PDF
Download- What is a hysteroscopy?
- What are the types of hysteroscopy?
- Why do I need a hysteroscopy?
- What can I expect before the procedure?
- What does the procedure involve?
- What are the risks?
- What can I expect after the procedure?
- What about going home?
- Are there any alternatives to having a hysteroscopy?
- Who can I contact with any concerns or questions?
What is a hysteroscopy?
A hysteroscopy is a procedure during which the inside of the uterus (womb) is examined using a thin narrow type tube called a hysteroscope.
The hysteroscope (2-5mm diameter) is carefully passed through the vagina, the cervix (neck of the womb) and enables the doctor to see into the uterus via the hysteroscope telescope. The images may be viewed on a computer monitor as the hysteroscopy is being done.
The procedure is most commonly carried out routinely in an out-patient clinic or as a day case procedure, meaning you will not be required to stay the night in hospital. It can help to give a clear diagnosis of problems you are experiencing and help to decide the right treatment for you.
What are the types of hysteroscopy?
The 2 types of hysteroscopy are:
Diagnostic hysteroscopy
To look for any abnormalities to the uterus and find the cause for any symptoms you may be experiencing.
Operative hysteroscopy
This is when a hysteroscopy involves an additional procedure to be done. This commonly means taking a biopsy (taking a small sample of tissue to be tested) or treating the symptoms you are having.
If your doctor thinks he/she may have to treat a condition or take a biopsy, he/she will discuss this with you and ask for your consent.
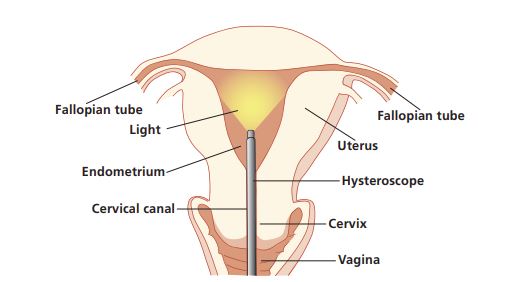
The hysteroscope is introduced through the cervical canal and into the uterus. No incision is necessary.
Why do I need a hysteroscopy?
A diagnostic hysteroscopy may be required to find the cause of various problems/symptoms you have been experiencing.
These can include:
- heavy or irregular vaginal bleeding
- post-menopausal vaginal bleeding
- unusual vaginal discharge
- for the diagnosis of womb cancer
- repeated miscarriages.
An operative hysteroscopy may involve removing:
- polyps (small lumps of tissue growing on the lining of the uterus)
- scar tissue and adhesions inside the uterus
- fibroids (non-cancerous growths)
- locate a ‘lost’/stuck contraceptive device
- ablate endometrium
- divide a septum
A contraceptive device may also be fitted immediately after having a hysteroscopy.
If extensive treatment is expected, an operative hysteroscopy may require you to have a general anaesthetic (when you are asleep). Arrangements will be made for this.
You should not have a hysteroscopy if you are pregnant, have a vaginal or urinary tract infection or if you are known to have cancer of the womb. Please inform nursing staff if you have any of these.
What can I expect before the procedure?
If you are having a hysteroscopy as an out-patient, you will not need any specific preparation but may have a local anaesthetic at the time of the procedure.
If you are required to come in for a day procedure you will have a pre-op assessment to discuss your hospital stay and explain your operation. Please do let us know about any concerns you have or if there is any information you think we should know about that will make your stay with us more comfortable.
You will need to make arrangements for your family, children or any other commitments that you have prior to coming into hospital and to cover the length of your recovery. You will see an anaesthetist and the doctor performing the surgery before you go to theatre. It is not unusual to feel anxious; the nursing staff will gladly discuss how you are feeling and talk you through your emotions.
What does the procedure involve?
A hysteroscopy is the same procedure whether you are awake or asleep.
A hysteroscopy is a similar sensation to having a smear test and should only last between 5-30 minutes.
The doctor may need to use a speculum inserted into the vagina to enable access to your cervix (similar to having a smear test) inserting the hysteroscope through the cervix into your womb. As the womb is small, gas or fluid may be introduced to make it larger. This helps the doctor visualise the lining of the womb, and any abnormalities, clearly. The camera at the end of the hysteroscope sends pictures from the inside of your womb to a video screen.
If a biopsy or treatment, is needed, other instruments will be passed into the womb and local anaesthetic will be used (numbs the area) to make the procedure less uncomfortable.
Once the procedure has been completed the doctor will gently remove the hysteroscope and speculum.
What are the risks?
As with any procedure, having a hysteroscopy comes with risks.
The main risks associated are:
Common risks:
- infection
- bleeding
Uncommon risks:
- damage to the womb
- damage to the bowel, bladder or major blood vessels
- infertility (very rare)
- failure to gain entry and complete intended procedure.
In order for you to make an informed choice about your procedure, please ask one of the doctors or nurses if you have any questions about the hysteroscopy before consenting.
What can I expect after the procedure?
If this procedure is as an out patient or you have had local anaesthetic, you may feel uncomfortable and numb. The effects will wear off. Take painkillers to help.
If you are having a general anaesthetic you may experience episodes of pain and/or nausea after the procedure. This is common. Please let the nursing staff know and they will assess you and take appropriate action. Your nurse will be checking your blood pressure, pulse, breathing and temperature and monitor for any vaginal bleeding.
Once you are fully awake you will be able to start drinking and eating.
What about going home?
If you are having this procedure as an out-patient or have had a local anaesthetic, you will usually be able to go home within an hour. You should feel well enough to walk, travel by bus or train –
or to drive home, providing you haven’t been given a sedative.
If you have had a hysteroscopy day case procedure you should be
able to go home within two – four hours post operatively.
Before you go home you need to have had something to eat, mobility checked and passed urine. When you go home, make sure you are not alone and someone can stay with you overnight. You will not be able to drive for 24 hours but this will depend on your ability to perform an emergency stop.
The anaesthetic is short-lasting. You should not have, or suffer from, any after-effects for more than two days after your procedure. During the first 48 hours you may feel more sleepy than usual and your judgement may be impaired.
You should not drink any alcohol during this time as it will affect you more than normal and you should not smoke. You should have an adult with you during this time and should not drive or make any important decisions or sign legal documents.
You should not use power tools, machinery or appliances that may cause harm.
Do not stand for long periods of time, or rise from a sitting to standing position too quickly as you may feel dizzy or faint. Tell someone, lay down flat and rest if this happens. You may experience some period-like cramps and bleeding. The bleeding is usually mild and should settle within seven days. To reduce the risk of infection you should use sanitary towels rather than tampons. Take it easy for the first one or two days and take painkillers as needed.
Please feel free to ask questions about your operation and recovery at any time.
Are there any alternatives to having a hysteroscopy?
Hysteroscopy is the gold standard investigation for abnormalities of menstruation but depending on your symptoms and circumstances it may be possible to examine your womb using:
Pelvic ultrasound
A technique that uses sound waves to produce an image of the inside of your womb.
Pipelle endometrial aspiration
When a narrow tube is passed through your cervix into your womb and suction is used to remove a sample of your womb lining.
Your doctor should explain all alternatives to you prior to having a hysteroscopy and explain why a hysteroscopy is necessary letting you have an open and informed choice of procedure.
Who can I contact with any concerns or questions?
If you have any problems or are worried, please do not hesitate to contact us on the gynaecology ward:
Royal Sussex County Hospital
Level 11 Telephone 01273 523191
Princess Royal Hospital
Horsted Keynes Telephone 01444 441881 Ext. 65686
This information sheet has been produced by the Gynaecology Ward Sister Hannah Tompsett and Samantha Backley.
This information is intended for patients receiving care in Brighton & Hove or Haywards Heath.
The information here is for guidance purposes only and is in no way intended to replace professional clinical advice by a qualified practitioner.
Publication Date: October 2021
Review Date: July 2024


