Your visit to the Outpatient Hysteroscopy Clinic
Download and print as a PDF
DownloadWhat is an outpatient hysteroscopy?
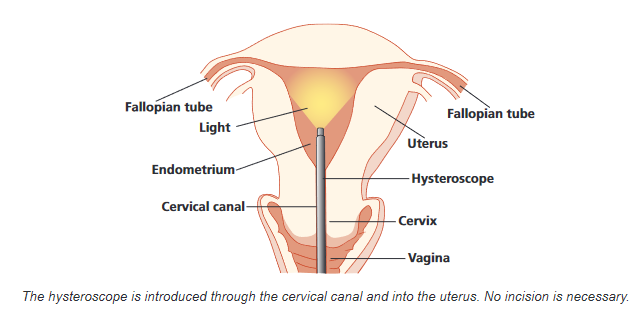
This procedure enables the Doctor or Specialist Nurse to examine the inside of your womb (uterus) and is done in an outpatient clinic whilst you are awake. A thin telescope like devise (hysteroscope) with a camera attached is passed through the neck of your womb (cervix). This enables the clinician to see whether there are any problems inside your uterus that may need further investigation or treatment.
An Outpatient Hysteroscopy is offered in order to give you the choice of having the procedure in the clinic awake therefore avoiding the need for a general anesthetic. You can choose the option that best suits you and your circumstances.
An Outpatient hysteroscopy usually takes between 10-15 minutes, although you will be booked for either a 30 minute or 40 minute appointment to allow for a discussion with the clinician first. You will be able to go home shortly after the procedure.
Why do I need a hysteroscopy?
You may have been referred for a hysteroscopy because you are experiencing symptoms such as:
- Heavy periods
- Bleeding in-between periods
- Irregular bleeding whilst on hormonal treatment
- Post-menopausal vaginal bleeding (bleeding after the menopause)
- Fertility concerns
- An ultrasound scan has detected a problem.
It may be possible to have a minor procedure done at the same time. This can include:
- An endometrial biopsy (taking a sample from the lining of the womb
- Removing a polyp (an overgrowth of the lining of the womb)
- Removing a small fibroid (benign growths of muscle and fibrous tissue)
- Insertion of a hormone releasing intrauterine device
- Removal of a coil from the womb when the threads are not visible
The purpose of this appointment is to find the cause of your problem and to plan or undertake the treatment needed.
How should I prepare for this clinic?
Taking pain relief, a short time before the procedure can lessen any discomfort you might feel. If you are not allergic or already taking them, you might like to take some paracetamol and ibuprofen about an hour before your procedure. Please follow the instruction on the packet about how much to take.
If you have been given a 40-minute appointment this is usually because you are going to have a polyp or small fibroid removed at the same time. You will be asked to arrive 30-minutes before your appointment time to be given further pain relief on your arrival. We advise that you don’t drive to a 40-minute appointment as the extra pain relief given might affect your ability to drive.
It is important there is no risk of pregnancy when the procedure is carried out. Therefore, we will ask your permission to carry out a pregnancy test before we start. Your hysteroscopy will be cancelled if there is a possibility that you might be pregnant.
As a precaution, it is advisable to use barrier contraception (like condoms) from the start of your period before the hysteroscopy and continue using them until after you have had the procedure.
Please eat, drink and take any regular medications as normal on the day of your procedure unless you have been advised otherwise.
If you are bleeding at the time of your hysteroscopy appointment, it is best that you still attend. Heavy bleeding, however, can make it difficult to do the procedure. If you have any concerns about this it is always best to ring the department to discuss. (Please refer below for contact numbers).
What can I expect during the Hysteroscopy?
Your appointment will start with a consultation. This will be with the doctor or nurse specialist performing your hysteroscopy. This is a good time for any questions or concerns you may have to be answered. It is important to us that you are involved in any decisions about your care and treatment.
The doctor or clinical nurse specialist will need to gain your consent before starting the procedure so you will be asked to sign a consent form if this hasn’t already been done in a previous appointment.
The actual hysteroscopy is then performed in a separate room with a nurse and healthcare assistant present to support you and assist the clinician during the procedure.
You will be asked to remove the bottom half of your clothing behind a curtain cubicle and to cover yourself with a paper sheet. You will then be required to lie down on an examination couch for the procedure.
A hysteroscope is then inserted through the cervix to give a clear view of the inside of your womb. Please note that a speculum may be used if you are having a local anesthetic, an endometrial biopsy or any treatment at the same time. Although no cuts are needed for the procedure, if you are having local anesthetic, this is given via an injection to the cervix. A fluid (saline solution) is used to allow the clinician to see clearly the inner lining of your womb and you may feel wet as it comes back out.
You will be talked through what is happening and able to see on a monitor along with the clinician. Pictures will also be taken as a record for your medical notes.
Please note that as you are awake if at any time you feel unable to cope with what is happening inform the staff and the procedure will be stopped.
What are the possible risks with Outpatient Hysteroscopy?
- Pain This can be either during or after the hysteroscopy. Any pain experienced is usually mild and like period pain. Simple pain relief can help with this. On occasion, women can experience severe pain
- Feeling or being sick or fainting This can affect a small number of women but usually settles quickly
- Bleeding This is usually very mild and lighter than a period. This normally settles within a few days and it is recommended that sanitary towels not tampons are used
- Infection This is uncommon and may present as a smelly discharge, fever or pain
- Failed / unsuccessful Hysteroscopy It may not be possible to pass the hysteroscope through your cervix into your uterus. This can be due to a tightly closed (stenosed) or scarred cervix
- Damage to the wall of the uterus (uterine perforation) This is rare and happens in less than 1 in 1000 hysteroscopy procedures but is slightly more common if someone has a polyp or fibroid removed at the same time. It occurs when a small hole is accidentally made in the wall of the uterus. This could cause damage to nearby tissues. It may mean you have to stay in hospital overnight. Usually the uterus will heal and nothing is done. However a further operation might be considered necessary to check for any damage and repair accordingly.
What can I expect after a hysteroscopy?
After the hysteroscopy your clinician will discuss with you whether any problems were found. If none are found, you may not need any follow up.
If an endometrial biopsy has been taken, a polyp or fibroid removed, then you will be sent a letter with the histopathology test results when they are available. This usually takes around 4-6 weeks.
You are encouraged to sit and rest for a few minutes in our recovery area and enjoy a drink before you go home.
You may experience some period like pain for 1-2 days. It is likely you will also have some spotting or fresh (bright red) bleeding that can last up to a week.
These symptoms usually settle very quickly, and most women feel able to go back to their normal activities on the same day.
It is advised that you refrain from sexual intercourse until the bleeding settles.
Who can I contact with any concerns?
If you have any concerns or are worried, please do not hesitate to contact our gynaecology wards:
Princess Royal Hospital:
Horsted Keynes Gynaecology Ward or clinic
01444 441881 Ext. 5686/5661
Royal Sussex County Hospital:
Level 11 Gynaecology Ward
01273 696955 Ext: 4022
This information is intended for patients receiving care in Brighton & Hove or Haywards Heath.
The information here is for guidance purposes only and is in no way intended to replace professional clinical advice by a qualified practitioner.
Publication Date: March 2021
Review Date: December 2023


