Overactive bladder
Download and print as a PDF
DownloadWhat is an overactive bladder?
Overactive bladder is a condition characterised by a number of symptoms, including:
- Urgency: having to rush to the toilet to pass urine.
- Frequency: need to pass urine frequently by day.
- Nocturia: waking up to pass urine.
- Urge incontinence: leakage of urine on the way to the toilet, if one is not quick enough.
The condition can cause considerable distress for patients and affect their quality of life. The fear of having to go to the toilet quickly makes patients look out for toilets all the time. This limits their activity and can lead to withdrawal and isolation. Having to wake up at night to pass urine can lead to disturbed sleep.
What causes overactive baldder?
Overactive bladder can be a manifestation of other diseases or conditions, such as:
- Diabetes mellitus.
- Urinary tract infection.
- Pressure on the bladder from an enlarged uterus or ovarian cyst.
- Local disease in the bladder, such as ulcer or mass.
- Neurological disease.
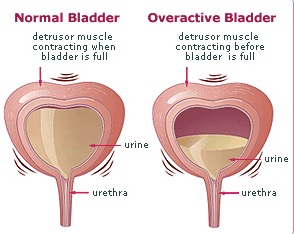
Having an overactive bladder can also be a problem in its own right, without an underlying cause. This happens when there is increased sensation from small volumes of urine in the bladder, with or without causing unwanted bladder contraction (spasm). Habitual frequent passing of urine for fear of leakage can lead to overactive bladder, as a learnt behaviour.
Overactive bladder
Excessive fluid intake, especially coffee, tea, cola and alcohol, as well as smoking, can irritate the bladder enough to cause or worsen the condition.
Overactive bladder can be experienced by patients with pelvic organ prolapse, where loss of support can lead to slipping down of the vagina and / or the uterus.
Overactive bladder may co exist with stress incontinence of urine (leakage of small drops of urine on coughing and sneezing), which is known as mixed incontinence.
It may also follow continence surgery, such as mid urethral tape sling operations and Burch colposuspension.
How is the diagnosis made?
The diagnosis is helped by completing a frequency volume chart (bladder diary).
An examination is carried out to identify underlying or contributory causes, such as neurological disease, enlarged uterus or pelvic organ prolapse.
Investigations to detect underlying problems include urine dipstick, culture and sensitivity and / or cystoscopy (camera examination of the inside of the bladder).
How is the condition treated?
If underlying or contributory cause(s) can be found, these should be corrected. For example, good control of blood sugar is important in diabetic patients and infection is treated with antibiotics.
If no specific cause can be found, then simple measures are attempted before moving to more complex and invasive lines of treatment.
Fluid advice: For the climate in the UK, a person is expected to drink 24ml / kg / day. This equates to about a litre and half to 2 litres (about 7 mugs or 10 cups) per day.
- Avoid inadequate fluid intake to minimise irritation of the bladder from concentrated urine.
- Avoid excessive fluid intake to reduce distension of the bladder and the need to go to the toilet frequently and / or quickly.
- Avoid or reduce caffeine containing drinks, such as coffee, tea, and cola, alcohol, fizzy drinks and acidic juices to reduce bladder irritation.
- Smoking cessation is also advisable.
Bladder training (drill): Trying to hold on for longer periods of time between visits to the toilet may help stretch the bladder. This will enable it to get used to holding larger volumes of urine. The trigger to go to the toilet can be suppressed by tightening the pelvic floor muscles. Patients can be referred for specialist physiotherapy to guide pelvic floor muscle training and bladder drill.
Medication: Tablets are available to reduce overactive bladder. These tablets can be taken once or twice daily. Some have fixed doses whilst the dose of others can be titrated according to response and side effects. A patch is also available. A gel is about to be introduced as well. Common side effects include dry mouth and constipation. The general practitioner will be able to offer one of these medications. It may be necessary to switch medication in the absence of an adequate response and or upon the occurrence of side effects.
These measures are tried for 4 to 6 months. If they don’t work, further tests are carried out.
These tests include:
- Urodynamic assessment to measure the pressure of the bladder as it is filled with fluid using a catheter (plastic tube).
- Cystoscopy (camera examination of the inside of the bladder).
Modern surgical measures include:
- Botulinum toxin: A bladder wall injection is given during cystoscopy to relax its muscle. This can be done under local anaesthesia and may need to be repeated.
- Percutaneous tibial nerve stimulation: A needle is inserted behind the ankle to stimulate the nerve at the back of the leg. This nerve shares the same centre with the bladder nerve supply. The stimulation will reduce bladder contraction and therefore overactive bladder. This treatment includes twelve half an hour weekly sessions.
More invasive measures include:
- Sacral neuromodulation: where needles are inserted in the back bone to suppress the nerve that controls the bladder.
- Clam cystoplasty: where a piece of bowel is used to enlarge the bladder diversion of urine into bowel.
These operations are more invasive and need to be considered carefully due to the potential for complications. They are reserved for extreme cases that do not improve with minimally invasive measures.
Who can I contact with any concerns or queries?
Please see below for contact telephone numbers.
Princess Royal Hospital: 01444 441881 Extension 5686
Royal Sussex County Hospital: 01273 696955 Extension 4013
Urogynaecology Unit at Lewes Victoria Hospital: 01273 474153 Extension 2178
Useful links
Your Pelvic Floor: Overactive bladder
www.patient.co.uk: Overactive bladder
This patient information leaflet was prepared by Dr. Sharif Ismail, Consultant Subspecialist Urogynaecologist.
This information leaflet has been approved at the Clinical Governance and Safety and Quality Meetings of the Department of Obstetrics and Gynaecology as well as Brighton and Sussex University Hospitals NHS Trust Carer and Patient Information Group (CPIG).
This information is intended for patients receiving care in Brighton & Hove or Haywards Heath.
The information here is for guidance purposes only and is in no way intended to replace professional clinical advice by a qualified practitioner.
Publication Date: May 2021
Review Date: February 2024


