Looking after a third or fourth degree tear following childbirth
Download and print as a PDF
Download- What is an injured perineum?
- How often do third and fourth degree tears occur?
- What will happen if I have a third or fourth degree tear?
- What’s the best way to care for my tear?
- Will it hurt when I go to the toilet?
- Will the tear affect my bowel control?
- How do I do my pelvic floor exercises?
- Will I be offered any physiotherapy?
- What should I do about sexual intercourse?
- What will happen at my follow up visit?
- Who can I contact for further information and advice?
- References
- Useful links
What is an injured perineum?
The perineum is the area of skin between the vagina and back passage (anus). Some women give birth without injury to the perineum. However, some may need episiotomy and some may have tears. Episiotomies can extend as well.
Tears can be classified into first, second, third and fourth degrees. First and second degree tears are injuries to the perineum which do not extend to the muscle of the back passage (anal sphincter).
First degree tears usually do not need stitches, unless there is excessive bleeding. A second degree tear will usually require stitching.
Third degree tears extend to the muscle of the back passage and a fourth degree tear also involves the linings of the rectum.
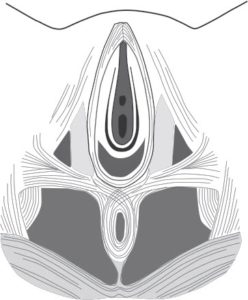
The perineum
How often do third and fourth degree tears occur?
Approximately three percent of women will have a tear extending to the back passage. However, these injuries cannot be predicted or avoided.
Research has shown that the risk of a third or fourth degree tear may be reduced by using perineal warm packs in the second stage of labour (see reference 1 below).
What will happen if I have a third or fourth degree tear?
These injuries are repaired by an experienced member of the obstetric team, in the operating theatre.
Following the repair to the anal sphincter muscle, antibiotics are prescribed for seven days, to reduce the risk of infection.
Regular painkillers will help keep you comfortable but can make you constipated, hence you will be encouraged to take laxatives.
It is important to take sufficient laxative to ensure easy passage of soft stools, but not so much that bowel control is a challenge. Sometimes this balance can be difficult to achieve, so do discuss this with your midwife if you are having any problems.
What’s the best way to care for my tear?
The first thing to do is look after yourself.
In the first 48 hours, rest as much as possible. Try lying on your back with your knees bent up, or lie on your side with a pillow between your legs.
Ice or perineal cold packs can help decrease pain and swelling.
Wrap ice cubes in a wet cloth (this protects the skin) and hold it next to the wound for up to 10 minutes. This is often easiest lying on your side. Cold shallow baths can also help reduce swelling and this in turn will promote healing. However, do not soak for longer than 10 minutes. It is better to avoid any cosmetic products in these baths.
It is important to keep the area clean, paying particular attention to washing with mild soap and warm water after a bowel action. Avoid using a sponge or flannel to wash around your stitches.
Dry the area carefully by patting dry with toilet paper, a soft clean cloth. Do not dry using the cold setting on a hairdryer. This dries up natural oils produced by the body.
When sitting for any length of time, especially when feeding, try to get comfortable and reduce the pressure on the area. You can try positioning cushions to support you or choose a firm chair and arrange a rolled up towel to support under the thighs. This reduces the pressure on the area of injury.
You can roll up a towel and place it in an upside down ‘U’ shape on the seat of the chair or roll two towels and place them in a ‘V’ arrangement. You could try some feeds when lying on your side with your baby next to you.
Will it hurt when I go to the toilet?
Avoid constipation, by eating a healthy balanced diet and drinking plenty of water. Try to keep an intake of 1.5 to 2 litres of fluid every day.
With laxatives and painkillers, bowel motion shouldn’t be painful but don’t rush things. It can be helpful for someone to care for the baby when you have your bowels open for the first time.
Things that can help include:
- A relaxed positioning on the loo can help make bowel movements easier. Sit comfortably on the toilet seat.
- Check that your knees are higher than your hips. A footstool or ‘toddler training stool’ may help.
- Rest your forearms onto your knees and lean forwards.
- Relax the pelvic floor muscles and stomach wall.
- Relax your jaw and try not to hold your breath.
- Holding a sanitary pad over the perineum can support this area and help you to feel more confident and comfortable when opening your bowels.
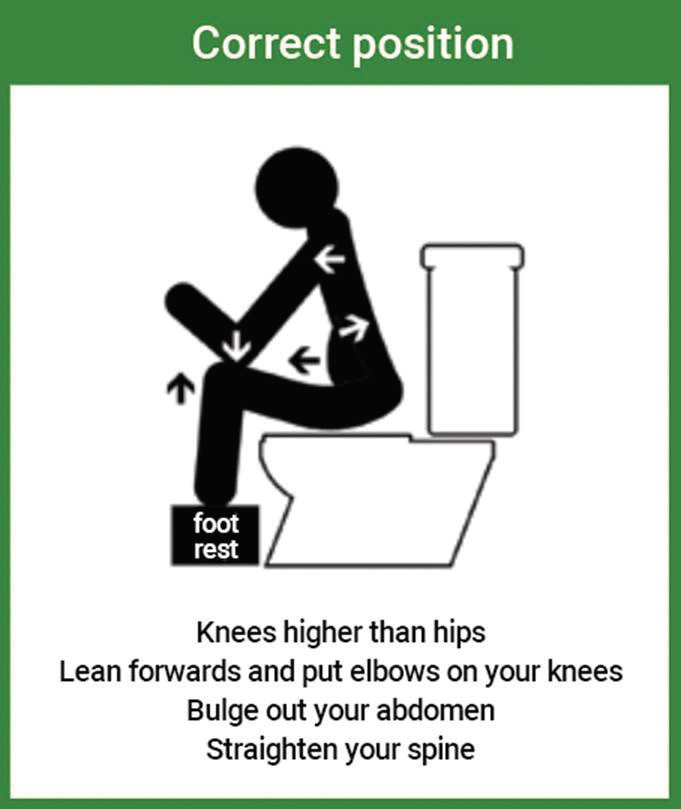
Opening your bowels
Will the tear affect my bowel control?
As a third or fourth degree tear affects the muscle of the back passage, some women develop problems with bowel control while the area is healing. Symptoms can include a feeling of urgency to empty the bowel, such that it is difficult to ‘hold on’. Wind control might be poor, leading to difficulty on wiping clean or incidents of diarrhoea.
Do be patient. Give the tissues time to heal and work to steadily strengthen the pelvic floor muscles. These are the muscles that support the pelvic organs and help bladder and bowel control. Therefore, it makes sense to work them back to strength after a difficult delivery.
Caffeine (coffee, tea and certain soft drinks) may make the need to open your bowels more urgent, hence plain drinks are better if bowel control is a challenge.
Work a little every day on pelvic floor exercises from the very first day after the birth, to help reduce the swelling and promote healing. Start gently.
You’ll be surprised that it won’t hurt! Over time, increased strength in these muscles will help restore good bowel control.
The exercises are detailed in the next section of this leaflet. If you should experience problems of bowel urgency, try tightening the muscles of the pelvic floor and the lower stomach wall gently, just a little, and aim to maintain this strength for a full 20 seconds to help control the urge and give you a little more time to get to the toilet.
How do I do my pelvic floor exercises?
Sit comfortably or rest lying on your side. These are good starting positions if these exercises are new to you.
- Close the back passage, as if you are trying to stop yourself from passing wind. Once you feel the back passage drawing in, try and work this feeling forward into the vagina, as if closing the urinary passage too. This feeling of ‘squeezing’ and ‘lifting’ internally is the basic pelvic floor contraction.
- The stomach muscles can also help the muscles of the pelvic floor to work. First of all, relax your stomach wall. Then gently draw in the lower part of your stomach wall towards your spine. Hold with easy effort and with easy breathing for a few seconds before letting go.
- Now try and work these two muscle groups at the same time. Pull up the pelvic floor muscles and draw in the lower part of the stomach wall. Feel the support these ‘core stability’ muscles provide to your pelvis and spine, and to the pelvic tissues.
It is important to do these exercises correctly.
Always try to work with easy effort and easy breathing: no jaw clenching or tightening your buttocks as you do these exercises.
Also try to feel how the muscles ‘let go’ when you stop working them.
Spend a little quiet time finding out how to work these muscles. Once you are sure that you are working these muscles correctly and once the soreness is settling, you are ready to start a strengthening programme.
Do ask your midwife to check that you are doing the exercises properly before you leave hospital. You should be given a more detailed postnatal exercise leaflet when you are discharged from hospital. It is usually given out in the discharge pack. If it is not in the envelope, you can ask your community midwife for a copy.
Remember!
You will need to build up to at least 30 tightenings a day, to strengthen weak muscles. The muscles do tire quickly in the early days, so don’t forget to rest for a short time between contractions.
As with all muscles, you can experience some soreness after you have worked well on strengthening exercises, so increase your programme gradually.
Try to fit the exercises around your activities throughout the day. Perhaps start the day with an exercise session before you get out of bed.
Repeat them as you get up and move around. It can help to link the exercises with something you do regularly: while feeding your baby, waiting for the kettle to boil, while cleaning your teeth, with a song on the radio.
You will need to think about bracing the pelvic floor and stomach muscles if you need to lift anything heavy. Try to keep the amount of lifting you do to a minimum, particularly in the early days after your baby is born, ideally lifting nothing heavier than your baby.
Delegate any heavier tasks while the tissues are healing and try not to stand for long periods of time.
Will I be offered any physiotherapy?
It is so important that you start working on daily pelvic floor exercises as a home programme.
The strength in these muscles can be assessed by internal examination. This will be offered as part of your follow up appointment.
You will be referred to a Specialist Women’s Health Physiotherapist to help and guide you in relation to pelvic floor exercises. The aim is to be seen at six weeks. You can contact Physiotherapy directly as well.
What should I do about sexual intercourse?
Once the bleeding has stopped and tissues have healed, you may resume sex when you feel ready. The timing of this is unique to every couple. It is understandable that the demands of feeding and broken nights, even without the added complication of stitches, may delay many couples from returning back to intimacy.
Do keep in mind that some of the stitches used to repair a third or fourth degree tear are meant to hold the anal sphincter muscle in a good position for a long time, to ensure its healing, and may not dissolve fully for 90 days.
For some new mothers, even with the best reassurance, it can take many months to feel confident about sexual intercourse. You could consider gently examining yourself first to see how comfortable the tissues feel. Sensitive tissues will become less tender over time when they are touched and gently stretched or massaged.
When you do resume intercourse, extra lubrication can be helpful and some positions will be more comfortable than others. Start gently and try to keep the pelvic floor muscles relaxed for initial penetration.
What will happen at my follow up visit?
To ensure full recovery, you will be offered an appointment to review your progress after the birth of your baby.
The repair will be checked, pelvic floor exercises progressed and any concerns that you have can be fully discussed.
A special information leaflet is available about this visit. It is posted with the clinic appointment letter and is also available online. Visit Your visit to the perineal clinic.
Your clinic appointment is usually made before you leave hospital. This is different from the six week review for you and your baby with your GP.
If you have suffered a third or fourth degree tear and do not have an appointment, do ask your midwife before you are discharged from the community visiting team.
If you need advice before your clinic appointment, you can contact your midwife up to 28 days after delivery. If you have been discharged by your midwife, then you can make an appointment to see your GP, to talk through any concerns.
We hope that you find this information reassuring and helpful.
Who can I contact for further information and advice?
Who can I contact?
If you have any problems or questions, you can contact the Postnatal Ward, the Physiotherapy Department or the Urogynaecology Unit.
Postnatal Ward at the Royal Sussex County Hospital:
01273 696955 extension 64392, 64793, or 64369.
Postnatal Ward at the Princess Royal Hospital:
01444 441881 extension 68480, 68478, or 68479.
Physiotherapy at the Royal Sussex County Hospital:
01273 523050
Physiotherapy at the Princess Royal Hospital:
01444 448664
Urogynaecology Unit at Lewes Victoria Hospital:
01273 474153 extension 2178.
References
1. Perineal Warm Packs: Dahlen et al., 2007
Useful links
This patient information leaflet was prepared by Dr. Sharif Ismail, Consultant Subspecialist Urogynaecologist.
This information is intended for patients receiving care in Brighton & Hove or Haywards Heath.
The information here is for guidance purposes only and is in no way intended to replace professional clinical advice by a qualified practitioner.
Publication Date: August 2021
Review Date: May 2024


