Having a bronchoscopy
Download and print as a PDF
DownloadThis information will help you and your family to understand more about bronchoscopy. Please read it and ask any questions you may have. The specialist will ask you to confirm that you have read it and explain the procedure to you personally, before asking you to sign a consent form. This will either be done in the clinic or in the endoscopy department immediately before the test. The leaflet is divided into sections:
- What is a bronchoscopy?
- Why do I need a bronchoscopy?
- Is there an anaesthetic?
- How is it carried out?
- Are there any risks?
- What happens afterwards?
- When will I know the results?
- What should I do on the day of the bronchoscopy?
- Who can I contact if I have a question?
- Where is the bronchoscopy performed?
What is a bronchoscopy?
Bronchoscopy is a test which allows inspection of the windpipe and smaller air passages of the lungs using a flexible camera about the size of a pencil.
Samples of fluid or tissue can be taken from inside the lungs and sent to the laboratory to check for any abnormalities.
Why do I need a bronchoscopy?
A bronchoscopy is usually suggested if a chest x-ray has shown some shadowing in the lung which is not clearing up, and which might indicate an underlying problem such as a cancer or an unusual infection. It is also helpful to look for the cause of any blood you may have coughed up. It can be used to retrieve a foreign body e.g. a peanut which has been inhaled. It is sometimes helpful in patients who have a chronic cough which has not been explained by simpler tests.
Is there an anaesthetic?
You do not need a general anaesthetic. A sedative injection may be given before the procedure starts. A local anaesthetic spray or gel is put into your nose where the flexible bronchoscope is to be inserted. More local anaesthetic is sprayed into your throat and more is given directly into the bronchial tubes through the bronchoscope as the examination progresses. No pain is felt from the inside of the lungs even if tissue samples are taken and the local anaesthetic is to help reduce any coughing.
How is it carried out?
You will be asked to lie on a couch, usually semi-upright, and the bronchoscopist (who is one of the doctors) will stand either in front of you to one side of the couch, or behind your head.
After any sedative injection and the local anaesthetic have taken effect, the bronchoscope will be passed gently into one side of your nose (occasionally your mouth), and back into your throat. The throat will be examined, more local anaesthetic applied and, after a pause to allow this to work, the bronchoscope will be passed down the windpipe and into the bronchial tubes. You will feel some discomfort as the bronchoscope is passed through your throat, which will pass, and after that the only uncomfortable feeling may be coughing.
The bronchoscope is small in relation to the windpipe and bronchial tubes and there is plenty of room to breathe, but you will not be able to talk. The images from the bronchoscope are transmitted to a TV screen which the bronchoscopist watches.
Samples are taken by squirting saline solution through the bronchoscope into the bronchial tube being examined and sucking back the liquid. The fluid is collected in special bottles. The saline now contains secretions from the lung which are analysed in the laboratory for signs of infection or cancer. Tissue samples, ‘biopsies’, are taken with tiny forceps passed through the scope and are sent to the lab for examination under the microscope.
In some conditions, it is necessary to take samples using an x-ray machine to guide the biopsies (trans-bronchial biopsies). If this is needed, the doctor will explain the process specifically beforehand. The procedure takes about 20 minutes.
Are there any risks?
Flexible bronchoscopy is very safe, but there are sometimes side effects and, rarely, complications which you need to be aware of in order to decide whether or not to agree to have this procedure.
Side effects
During the examination, coughing is common, though local anaesthetic is used to reduce this as much as possible. After the test, it is likely that you will have a sore throat for a day or two or some soreness of the nose. You might also have a hoarse voice for a short time.
It is quite common to cough up small amounts of blood for a few hours after bronchoscopy especially if biopsies have been taken. Nose bleeds can occur but are quite rare. You should tell the doctor if you get troublesome nose bleeds and if they affect one side of your nose in particular so that the bronchoscope can be inserted through the other nostril.
Complications
Major complications are uncommon, affecting 1– 5 patients per 1000 bronchoscopies. These include significant bleeding or collapse of the lung following a biopsy, infection in the lung or an allergic reaction to local anaesthetic or sedative.
An irregular or rapid heart rhythm may occur in patients with underlying heart disease.
Breathing difficulties can occur during bronchoscopy in patients who have bad asthma or COPD (chronic obstructive pulmonary disease, such as emphysema) and the effect of sedation may reduce breathing further and cause low oxygen levels in the blood. Very rarely this is severe enough to require an anaesthetist to insert a breathing tube through the mouth into the windpipe and transfer to an intensive care unit.
Even more rarely, cardiac arrest and death can occur. Such devastating complications are extremely uncommon, reportedly once per 10,000 bronchoscopies, but the risk is greater if there is already serious lung or heart disease present and is taken into account in weighing up the pros and cons of having the test when discussing it with you.
Your safety
To reduce the risk of complications, your lung function (breathing capacity) and oxygen levels will be checked in the clinic. Blood tests will be done to check blood clotting to reduce the risk of unexpected haemorrhage. It is important that you have told the healthcare team of any breathing or heart problem you have, of any allergies that you know of, and what medicines you are taking. During the procedure your oxygen level will be continuously checked via a clip-probe on your finger, and you may be given extra oxygen through a mask or nasal tube. Your heart will be monitored and your blood pressure taken at regular intervals.
What happens afterwards?
After the bronchoscopy you will be taken back to the recovery area a few yards away from the bronchoscopy room. For 2 hours the nurses will check your pulse, blood pressure and breathing at intervals. During this time you will not be able to eat or drink due to the numbness in your throat.
We do not routinely discuss the results of the examination with you before you go home. This is because any sedative injection often makes it hard to remember things for a few hours, but also because often we won’t yet know the answers until the lab results are back. If there is important information to tell you, and you are with someone, then we are happy to tell you what we have found.
You will normally be allowed home after 2 hours. You must not drive yourself, and should not drive or operate machinery for 24 hours. You should have someone at home with you until the following day, and should take it easy for 24 hours.
You should not drink alcohol and you should not sign any important documents during this time. All of this is to make sure that the effects of the sedation have completely worn off.
When will I know the results?
You will be given an outpatient appointment a week or two after the bronchoscopy to discuss the results. It is possible that other x-rays or scans may be needed first and the doctor will explain if this is necessary.
What should I do on the day of the bronchoscopy?
Eating and drinking
You should not eat anything at all for at least 6 hours before the test. You can drink water only (no tea, coffee, or other liquids) for up to 2 hours before. For the final 2 hours before the test you should not eat or drink anything at all.
Medication
You should take your usual medications on the morning of the test, with any necessary sips of water, except:
Warfarin: usually stopped 5 full days before the procedure. You will need an INR blood test 1-2 days before the procedure to ensure you INR is below 1.5. In some situations, we may give you an alternative shorter acting agent to take instead, in the lead-up to your procedure.
Aspirin: Do not take on the morning of the procedure.
Clopidogrel: Usually stopped 7 full days before the procedure.
Dipyridamole: Usually stopped 7 full days before the procedure.
Ticagrelor: Usually stopped 7 full days before the procedure.
Rivaroxaban: Usually stopped 2 full days before the procedure.
Apixaban: Usually stopped 2 full days before the procedure.
Dabigatran: Usually stopped 2 full days before the procedure.
Dalteparin: (injections) Usually stopped 1 full day before the procedure.
Enoxaparin: (injections) Usually stopped 1 full day before the procedure.
Travel
Please arrange for someone to bring you and take you home. The hospital can only provide transport if it is impossible for you to make any suitable arrangements.
Reporting for the bronchoscopy
Report at the time you have been given in the clinic.
The nurses will show you to a bed and check your details. You will be asked to change into a hospital gown, and your pulse, blood pressure and oxygen levels will be recorded. A small plastic cannula will be placed in one of your arm veins, to be used for any sedative injection later. The doctor who is going to carry out the bronchoscopy will talk to you about the test, make sure you understand what will happen and that you have read this leaflet, and then ask you to sign a consent form.
Who can I contact if I have a question?
If you have a question about the bronchoscopy, contact one of the respiratory administrators on 01273 696955, extension 67825.
In the very unlikely event that you have a problem after going home from the test you will need to contact the respiratory administrators (details above) if within normal working hours, or the medical registrar on call if out-of-hours, either at:
Royal Sussex County Hospital on 01273 696955 or
Princess Royal Hospital on 01444 441881
Further information and support: The British Lung Foundation, helpline 03000 030 555.
Where is the bronchoscopy performed?
At the Royal Sussex County Hospital, the bronchoscopy takes place on:
Endoscopy Unit
Level 9
Millennium Building
Royal Sussex County Hospital
Eastern Road
Brighton
BN2 5BE
The Millenium Wing can be seen on the map below:
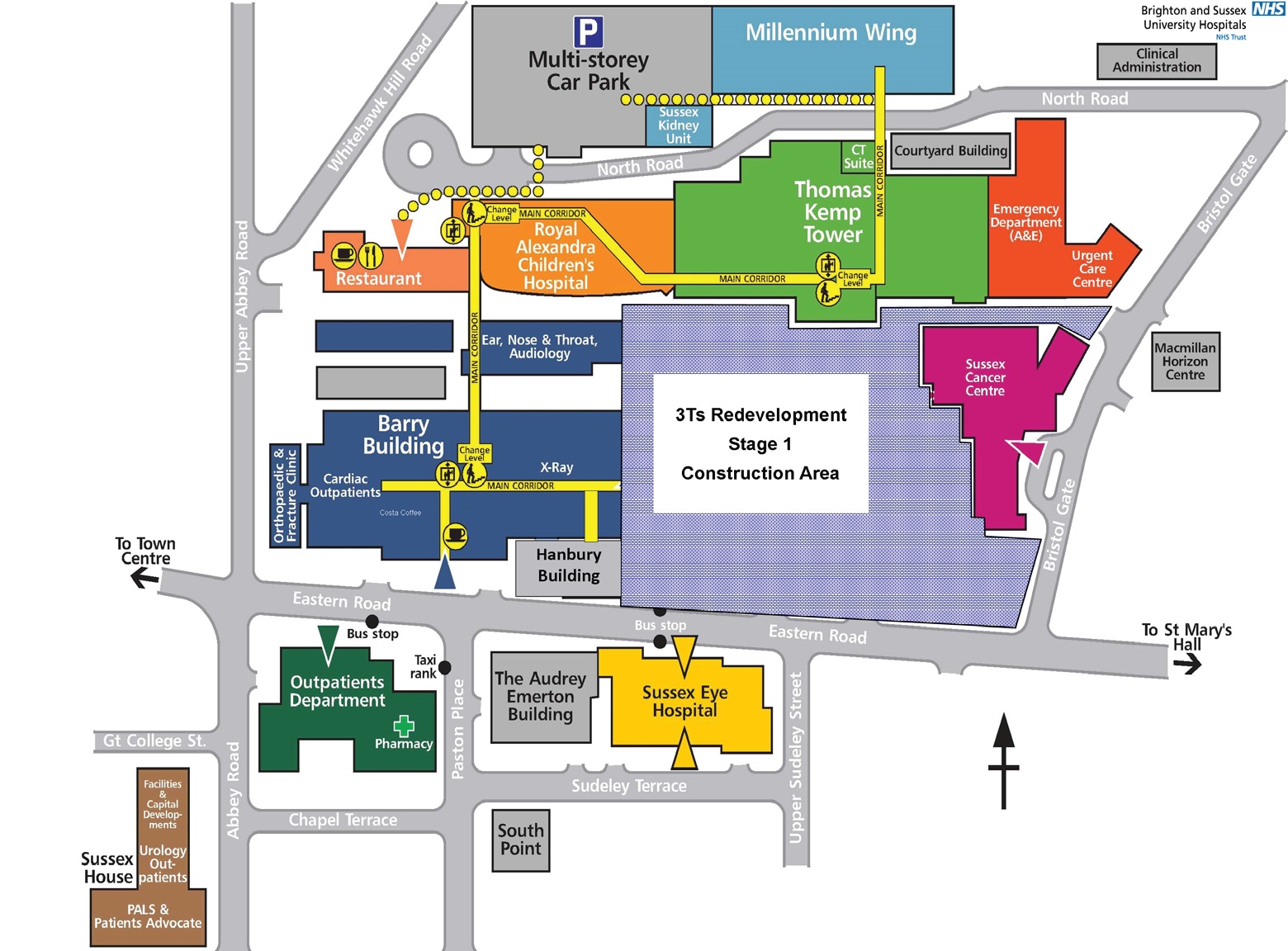
Brighton site map
At the Princess Royal Hospital, the bronchoscopy takes place on:
Cuckfield Ward
First floor
Princess Royal Hospital
Lewes Road
Haywards Heath
RH16 4EX
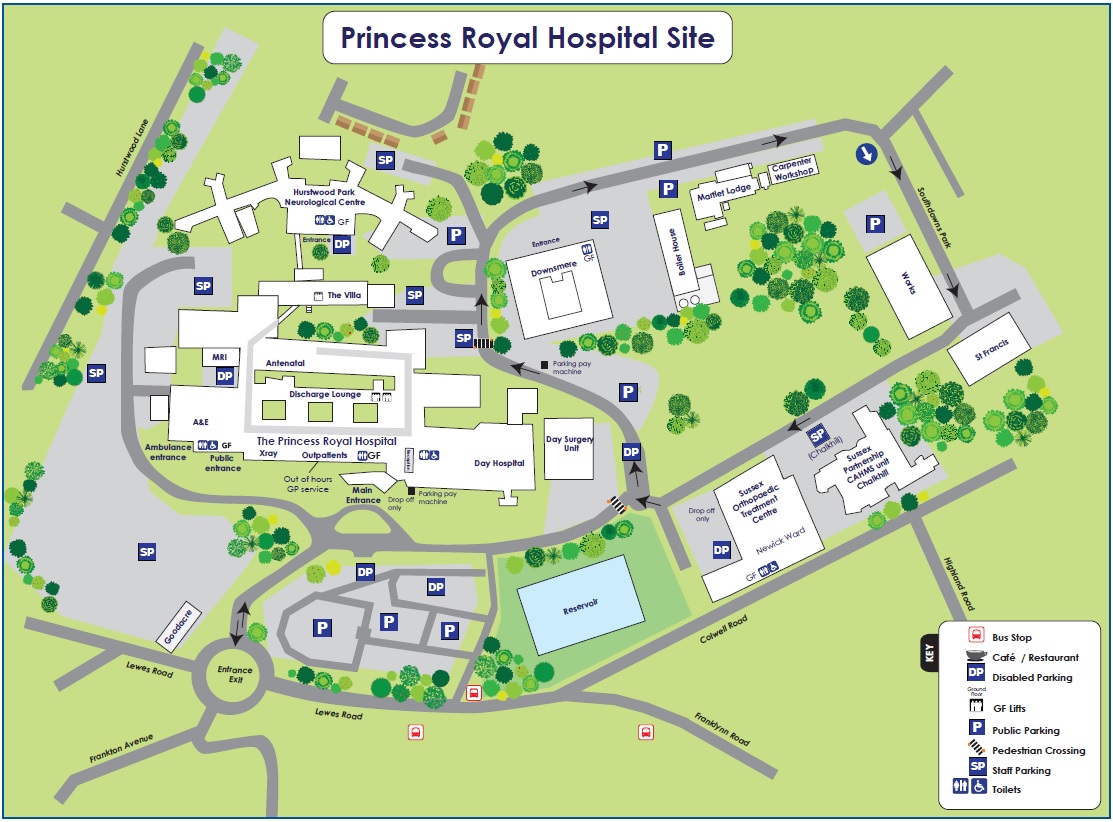
Princess Royal Hospital site map
The information here is for guidance purposes only and is in no way intended to replace professional clinical advice by a qualified practitioner
Publication Date: December 2021
Review Date: September 2024


