Edge to edge mitral valve repair PASCAL procedure
Download and print this article
DownloadValvular heart disease
Your heart is a muscle which pumps blood to your lungs and around the rest of your body. There are four valves in your heart. Normally, these valves open to let blood flow through or out of your heart, and then shut to keep it from flowing backwards.
If your valve is diseased or damaged this can affect the flow of blood to your heart in two ways:
- If the valve does not open fully, it will obstruct the flow of blood. This is called valve stenosis
- If the valve does not close properly, it will allow blood to leak backwards, in the wrong direction. This is called valve incompetence or regurgitation.
What are the symptoms?
The symptoms of valvular disease vary depending on which valve is affected, they may include:
- Tiredness or breathlessness when exercising
- Palpitations or feeling like your heart is racing.
The back pressure (the effect of blood flowing backwards) can also cause shortness of breath and swelling of the ankles and legs.
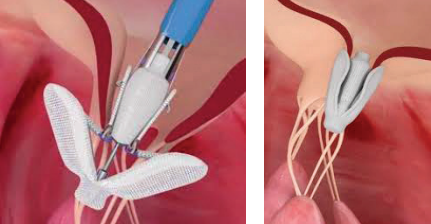
Edge to edge mitral valve repair using PASCAL
For people with mitral valve regurgitation, one way of treating their heart problem is to repair the leaking valve using a minimally invasive technique called Edge to Edge repair. During this procedure a thin flexible tube, called a catheter is introduced into the body via a vein in your groin/upper leg. The PASCAL device is then introduced into the body using this catheter and is positioned on the mitral valve holding or ‘clipping’ the
leaflets together in a way that reduces the leakage. The PASCAL procedure is carried out under a general anaesthetic but is a less invasive way to repair the mitral valve and does not involve open-heart surgery or cutting the chest bone.
You will need to have a number of tests to see if the PASCAL procedure is the right one for you. These tests will include a transthoracic echocardiogram (ultrasound scan of the heart) and/or a transoesphogeal echocardiogram (TOE). A TOE is another way of carrying out an ultrasound where a flexible tube is passed down your throat to obtain more detailed images. This is done under heavy sedation. A TOE takes approximately 20–30 minutes.
Prior to admission for the PASCAL procedure you will be contacted by a member of our admissions team who will advise you of your procedure date.
You may also be contacted by our Structural Heart Nurse Specialists to attend a pre-admission clinic or be approached about participating in a clinical trial.
The Structural Heart Nurse will advise you about taking your warfarin/blood thinners prior to admission.
What are the risks and benefits?
The PASCAL procedure has a good success rate. The potential benefits are improved heart function, a better quality of life and perhaps an increased life expectancy.
However, as with any heart procedure there are risks, and they vary from person to person. This will be discussed by your cardiologist when you come for your appointment at the clinic and again when you come to sign the consent form.
After the procedure
The procedure lasts approximately 2-3 hours. We will close the puncture site in your groin with a small suture. Once the procedure has finished you will wake up while still in the theatre and then be transferred to our Cardiac Care Unit (CCU), where you will stay for at least 12hrs.
The nurse looking after you will regularly inspect this wound when you are back on the ward.
We will observe your heart rhythm on a cardiac monitor overnight. If all is well, you will be able to sit up on return to ward and get out of bed that evening or the following morning.
While you are in the Cardiac Care Unit (CCU) it may not always be possible to care for you with other patients who are the same sex as you because we will be using specialised equipment as part of your care. However we provide substantial screening around your bed, to preserve your privacy and dignity. There is limited space in the ward, so we suggest you do not bring too many things with you into hospital.
Before you go home we will review your medication. You may need to take some blood thinning medication. Your doctor will review your history and advise if other medications need stopping or the dose altering.
Going home
If you are recovering well, you will be able to go home the day after your procedure.
We recommend that you have someone who can stay with you for up to 2 days following discharge to help with recovery.
If you cannot organise your own transport home, then please contact us prior to admission as soon as you can.
Wound care
It is normal for your groin to feel tender for a few days after the procedure. A bruise may develop with discolouration down as far as your knee.
The wound may be covered in a clear film dressing. This can be peeled off when you get home. The wound area should be kept clean and dry as normal. We also advise you to avoid hot baths for 48 hours after discharge as this may encourage bleeding.
If you develop a hard tender lump under the skin around the wound, please contact CCU on 01273 696955 Ext.64484. This may be the result of a collection of blood under the skin.
In the highly unlikely event of your wound starting to bleed, lie down and apply pressure to your groin for a few minutes. Call CCU for advice if you are unsure.
Recovery at home will continue at different rates for each person. It may a few weeks or months to feel the maximum benefit following the PASCAL procedure.
Activity
We advise you not to do anything strenuous for the first week after returning home. Avoid lifting heavy objects (e.g. shopping, suitcases) excessive pulling and pushing (e.g. cutting the grass, digging the garden, shoveling and vacuum cleaning).
Give yourself a few days to get your strength back before returning to your everyday activities. A good starting point is to take regular walks on a daily basis. You don’t have to avoid climbing stairs or walking up hills - just take them slowly and steadily at first. In time, you will find that you can do more than you could before.
Returning to work
This will depend on many factors such as the overall state of your health and the type of work that you do.
You may like to discuss this in more detail with your cardiologist or GP.
Travel
Government rules say that you are not allowed to drive for 4 weeks following your PASCAL procedure. You don’t need to let the DVLA know unless you hold a commercial licence.
It’s safe to fly 2 weeks after your PASCAL procedure - assuming you have not had any complications and you are the passenger and not the pilot! However, its best to check with your airline as each has its own procedure.
Hospital follow-up
You will be invited back to see your Structural Heart Team for a review. This will usually be 2-3 months following discharge. Thereafter you will return to the care of your referring hospital, if you live outside the Brighton area.
If you have any questions, queries or concerns please do not hesitate to contact our Structural Heart Specialist Nurses –
Patrick Mejia and Manuel Pellegrino, Mobile: 07769 286982
Email: uhsussex.structuralheartnurses@nhs.net
Useful telephone numbers/websites
Structural Heart Nurse Specialist
Patrick Mejia and Manuel Pellegrino
Mobile: 07769 286982
Email: uhsussex.structuralheartnurses@nhs.net
Cardiac Care Unit
01273 696955 Ext.64484
Cardiac Research Team
Telephone: 01273 696955 Ext.64049
British Heart Foundation
Helpline: 0300 330 3311
Email: hearthelpline@bhf.org.uk
Website: www.bhf.org.uk
Heart Valve Voice
Website: www.heartvalvevoice.com
This information is intended for patients receiving care in Brighton & Hove or Haywards Heath.
The information in this leaflet is for guidance purposes only and is in no way intended to replace professional clinical advice by a qualified practitioner.
Publication Date: February 2022
Review Date: November 2024

