Cystoscopy
Download and print as a PDF
DownloadWhat is cystoscopy?
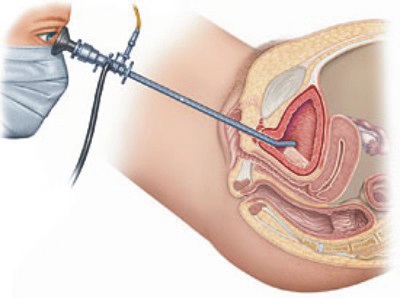
This is an operation carried out to examine the inside of your bladder (water works) and urethra (pipe that takes urine out). The operation is carried out using an endoscope (camera) that goes inside the bladder and urethra (pipe that takes urine out).
Why do I need a cystoscopy?
This operation is needed in a number of conditions;
- When patients have pain in their bladder to detect any ulceration or bleeding, commonly known as painful bladder syndrome.
- Patients with frequency and / or urgency of micturition as well as urge incontinence (leakage of urine on the way to the toilet) who do not improve on fluid advice, bladder training and / or medications, to pick up abnormalities such as stones and / or tumours.
- Patients with difficulty passing urine to detect stricture (narrowing) or diverticula (side pouching) of the urethra (pipe that takes the water out).
- When patients suffer from frequent urinary tract (water works) infection to rule out any abnormality (especially diverticula, which is side pouching of the bladder and / or stones).
- When there is blood and / or abnormal cells in the urine to rule out any abnormality (especially cancer).
- Patients with continuous involuntary leakage of urine to detect urinary fistula (hole connecting between the water works and front passage).
What can I expect before the operation?
At your pre op assessment and on your admission day the nurse will go through your hospital stay and explain your operation. Please do let us know about any concerns you have or if there is any information you think we should know about that will make your stay with us more comfortable.
You will need to make arrangements for your family, children or any other commitments that you have prior to coming in to hospital and to cover the length of your recovery.
You will see an anaesthetist and the doctor performing the surgery before you go to theatre. It is not unusual to feel anxious; the nursing staff will gladly discuss how you are feeling and talk you through your emotions.
If you have not already completed a frequency volume chart and quality of life questionnaires, you might be asked to do so before surgery. Likewise, if you have not already signed the consent form on booking, the doctor will go through it with you before you go to theatre.
You might be asked for permission to enter your data on the national database for continence and prolapse surgery. This is a quality control measure to compare the safety and effectiveness of such procedures at the hospital against other units in the country. You might be given a frequency volume chart and quality of life questionnaires to complete and bring with you as you attend for follow-up after surgery. This will enable assessing the benefit of surgery for you.
What does the operation involve?
The operation is commonly done while you are awake, using local anaesthesia, though it can be done while you are asleep.
Local anaesthesia may be inserted on the ward. It is introduced into the bladder through a catheter (small tube) under lubrication. You will be asked to lie on your tummy for five minutes, on each of your side for five minutes and on you back for five minutes.
The area around the urethra (pipe that takes urine (water) will be cleaned and you will be covered with drapes. The camera is introduced and you will be able to see on the screen, if you wish. The urethra and bladder are inspected systematically to detect any abnormality. A biopsy might be taken from any suspicious area(s), as required. The operation takes about 10 to 15 minutes.
Cystoscopy
What are the risks?
There are risks with any operation but these are small. The main risks associated with cystoscopy are:
Common risks:
- Burning micturition. Should settle within a day or two.
- Urinary tract infection, which may need antibiotics. Drink more water than you usually do for the first few days after the operation, to flush the bladder. If you are at risk of infection, for example diabetic, you might be given prophylactic antibiotics.
- Postoperative pain.
- Blood stained urine this should settle within a day or two.
- Frequent and / or urgent need to pass urine, which may be accompanied by leakage on the way to the toilet. This may need oral medication to calm down the bladder muscle.
Uncommon risks:
- Venous thrombosis and pulmonary embolism (clot in leg / lung). These are extremely unlikely after this minor procedure.
In order for you to make an informed choice about your surgery please ask one of the doctors or nurses if you have any questions about the operation before signing the consent form.
What can I expect after the operation?
If you have the operation under anaesthesia, you may experience episodes of pain and / or nausea, as you come round. Please let the nursing staff know and they will assess you and take appropriate action.
The doctor will explain the findings and the next step in the management of your condition(s). You will be able to go home shortly after the operation.
What about going home?
Most patients go home on the day. As you physically recover from your operation, the nursing team will discuss your convalescence. To ensure you have a good recovery you should take note of the following:
Rest: During the first day or two at home it is common to feel tired. You should tailor your activity to your ability but you should be back to normal within a few days.
Blood stained urine: This is caused by passing the camera into your bladder and usually subsides within a day or so.
Housework: Tailor your activity to your ability but you should be back to normal within a week.
Exercise: You should be able to resume your usual exercise activity within a week.
Diet: A well balanced nutritious diet with high fibre content is essential to avoid constipation. Your bowels may take some time to return to normal after your operation and you may need to take laxatives. You should include at least five portions of fruit and vegetables per day. You should aim to drink at least two litres of water per day.
Sex: You should usually allow a week or two after the operation.
Returning to work: You should be able to return to work within a week.
Driving: It is usually safe to drive after few days but this will depend on your level of concentration and ability to perform an emergency stop and your car insurance company agree.
What about follow up?
The doctor who will see you after the operation will discuss this with you. You may not need a follow up, depending on the reason you are having the operation and its findings. If you need one, it will be arranged. If you have problems before this you can either contact your doctor or contact the hospital to bring the appointment forwards.
You might be given a frequency volume chart and quality of life questionnaires to bring back with your for follow up. In addition to helping the evaluation of your condition after the operation, the data will be added to the national database for continence and prolapse surgery. This is a quality control measure, to compare the outcome of the operations carried out at the hospital against the rest of the country.
Who can I contact with any concerns or questions?
You should contact your doctor or the hospital if you notice increased temperature, frequent micturition, smelling or cloudy urine or generally unwell.
If you have any problems or questions, you can contact:
Princess Royal Hospital, Horsted Keynes Ward: 01444 441881 extension 5686
Royal Sussex County Hospital, Level 11: 01273 523191 extension 4013
Urogynaecology Unit at Lewes Victoria Hospital: 01273 474153 extension 2178
References and useful links:
This leaflet is intended for patients receiving care in Brighton & Hove or Haywards Heath.
This patient information leaflet was prepared by Dr. Sharif Ismail, Consultant Subspecialist Urogynaecologist.
This information leaflet has been approved at the Clinical Governance and Safety and Quality Meetings of the Department of Obstetrics and Gynaecology as well as Brighton and Sussex University Hospitals NHS Trust Carer and Patient Information Group (CPIG).
Ratified April 2017 Women’s Safety and Quality Committee.
Disclaimer
The information in this leaflet is for guidance purposes only and is in no way intended to replace professional clinical advice by a qualified practitioner.
Publication Date: May 2021
Review Date: February 2024


