Autologous sling
Download and print as a PDF
Download- What is an autologous sling?
- Why do I need an autologous sling?
- What can I expect before the operation?
- What does the operation involve?
- What are the risks?
- What can I expect after the operation?
- What about going home?
- What about follow up?
- Are there any alternatives to having an autologous sling?
- Who can I contact with any queries or concerns?
What is an autologous sling?
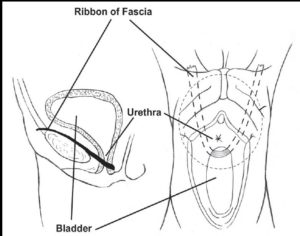
An autologous sling is an operation where a ribbon of fascia (fibrous tissue strip) is taken from one of the abdominal wall layers and placed underneath the urethra. This strip is passed on either side to be fixed back to the abdominal wall. This acts like a hammock to support the urethra. It can be performed under general or regional anaesthetic, such as a spinal anaesthetic.
Autologous sling
Why do I need an autologous sling?
An autologous sling is used for the treatment for stress incontinence of urine, which refers to leakage of urine on coughing and sneezing. Surgery is carried out when conservative measures, including pelvic floor muscle training, have failed. The operation is intended to support the urethra to avoid leakage of urine.
What can I expect before the operation?
At your pre op assessment and on your admission day the nurse will go through your hospital stay and explain your operation. Please do let us know about any concerns you have or if there is anything you think we should know about that will make your stay at the hospital more comfortable.
You will need to make arrangements for your family, children or any other commitments that you have prior to coming in to hospital and to cover the length of your recovery.
You will see an anaesthetist and the doctor performing the surgery before you go to theatre. Completing a frequency volume chart and quality of life questionnaire at follow up will enable assessing the benefit of surgery for you You will be asked to sign a consent form, if you have not already signed one.
You will be asked for permission to enter your data on the national database for continence and prolapse surgery. This is a quality control measure to compare the safety and effectiveness of such procedures at the hospital against other units in the country.
It is not unusual to feel anxious, the nursing staff will gladly discuss how you are feeling and talk you through your emotions.
What does the operation involve?
The operation is done through a small cut across the abdomen, which will not show above the bikini line. A strip of fascia is obtained from your abdominal wall and secured with a permanent suture on either end. Each end is than passed alongside the urethra, through an incision in the vagina, to be fixed back to your abdominal wall. The wounds in the abdomen and vagina are then closed. You may have a catheter inserted to drain your bladder which should be removed within 24 hours.
What are the risks?
There are risks with any operation but these are small.
Common risks that can happen with this operation:
- Initial difficulty in passing urine. This is usually managed by leaving the catheter to drain the bladder for longer. You may go home with a leg bag for few days. Patients may need to use clean intermittent self catheterisation for a short period of time. In extremely rare circumstances, patients may need to have the operation undone to help them pass urine properly.
- Postoperative pain.
Uncommon risks:
- Overactive bladder symptoms such as frequent and urgent need to pass urine may persist or develop, this can be managed with medication.
- Urinary tract infection, which may need antibiotics.
- Wound infection, which may need antibiotics.
- Wound bruising and delayed wound healing.
- Damage to the bladder and / or bowel, which will be repaired at the time. If such injury is not identified and repaired at the time, there is a risk of fistula, but this is extremely rare.
- Venous thrombosis and pulmonary embolism (blood clot in leg or on the lung), You will be given elastic stockings and / or injections to prevent these clots.
- Failure to improve or cure stress incontinence or its recurrence with time. This will require re assessment and may necessitate repeat surgery.
- Late onset difficulty passing urine. This can happen days or even weeks after being able to pass urine smoothly. The management is the same as initial difficulty passing urine, either by using a catheter with a leg bag and / or clean intermittent self catheterisation.
- Hernia at site of entry across the abdomen.
- Haemorrhage requiring blood transfusion.
- Return to theatre because of bleeding.
In order for you to make an informed choice about your surgery please ask one of the doctors or nurses if you have any questions about the operation before signing the consent form.
What can I expect after the operation?
As you come round from the anaesthetic, you may experience episodes of pain and / or nausea. Please let the nursing staff know and they will assess you and take appropriate action. A small drain may be placed in the abdominal wound to remove any excess blood. You may have a catheter in the bladder, until you are fully mobile after the operation.
You will have a drip to give you fluids, though you will be able to eat and drink. You may have a PCA (Patient Controlled Analgesia) pump to control your pain. This is not common and will be discussed with you before the operation by the anaesthetist. The nurses will assess you regularly to ensure that the PCA is effective. We will use a pain score to assess your pain 0 to 10; 0 = No Pain, 10 = Very Strong Pain.
Your nurse will be checking your blood pressure, pulse and breathing.
They will also be monitoring your temperature, the wounds and any vaginal bleeding. They will also ask you to move from side to side and to do leg and breathing exercises once you are able, this will help prevent any pressure damage, a DVT (deep vein thrombosis) or chest infection.
The first 12 hours after the operation: You can expect pain and discomfort in your lower abdomen for the first few days after the operation, which can be treated with paracetamol or stronger pain killers if you need them.
Day 1 after the operation: The drain, drip and catheter are usually removed within 24 hours. The nursing staff will assist with washing as necessary and encourage early mobilisation. We would normally expect you to sit out of bed and begin to walk around the day after your operation.
You will be able to go home when you are passing urine without difficulty. You will be asked to pass urine in a jug and will have a scan to measure how much urine is left in the bladder.
You will have a dressing on the wound that will be removed the day after your operation and you will be able to shower. You may also find it difficult to open your bowels at first, we will give you mild laxatives to soften your stools and prevent constipation and straining.
Exercise: Exercise is important and it is advisable to go for short walks each day, increasing the distance gradually. You should avoid straining or heavy exercise for 3 months. You may return to light exercise, like gentle swimming and cycling after 4 to 6 weeks. You will be able to manage the stairs on your arrival home. We encourage you to do pelvic floor exercises to enhance muscle tone.
Diet: A well balanced nutritious diet with high fibre content is essential to avoid constipation. Your bowels may take some time to return to normal after your operation and you may need to take laxatives. You should include at least 5 portions of fruit and vegetables per day. You should aim to drink at least 2 litres of water per day.
Returning to work: This will depend on the nature of your work. If you work in an office based environment, you will need 4 to 6 weeks off work. If your work involves lifting and exertion, you will need up to 3 months off work. The hospital doctor will provide a sick note for this period.
Driving: It is usually safe to drive after 6 weeks but this will depend on your level of concentration and ability to perform an emergency stop and your car. It is wise to check your insurance policy.
What about going home?
You will be seen and assessed the following day to check on your recovery. Decisions will be made about your care and you will be kept informed on a daily basis. Please feel free to ask questions about your operation and recovery at any time.
The average length of stay following autologous sling is 1 to 2 days. In most instances, you can go home the following day. As you physically recover from your operation, the nursing team will discuss your convalescence.
To ensure you have a good recovery you should take note of the following:
Rest: During the first two weeks at home, it is common to feel tired, exhausted and emotional. You should relax during the day gradually increasing the number of things you do each day. Avoid crossing your legs when you are lying down.
Vaginal bleeding: You can expect to have some vaginal discharge or bleeding for a few days after surgery. This is like a light period and is red or brown in colour. Sanitary towels should be used rather than tampons, to reduce the risk of infection.
Stitches: The wound across your abdomen will be closed by dissolvable stitches. If after 7 days you notice the stitches have not dissolved, then they will need to be removed. This is normally done by your practice nurse and you will need to make an appointment. We advise that you shower daily and keep the wound clean and dry. There is no need to cover the wound with a dressing. The stitches in your vagina are also dissolvable and the knots should fall out on their own.
Housework:
Weeks 1 to 2: we recommend that you do light activities around the house and avoid any heavy lifting (not more than 1.5kgs in each hand).
Weeks 3 to 4: we recommend that you gradually introduce lighter household chores, dusting, washing up, making beds and ironing. You may begin to prepare food and cook remembering not to lift any heavy items.
Weeks 4 to 6: By this time you should resume normal daily activities, but continue to refrain from straining until 3 months after surgery, to allow the sling to heal fully.
Intercourse: You should usually allow 4 to 6 weeks after your operation, to allow the vaginal scar to heal. If you experience vaginal dryness, you may wish to try a vaginal lubricant from your local pharmacy. If after this time you are experiencing pain or any problems with intercourse then you should see your GP.
What about follow up?
You will be invited for follow up, usually about 8 weeks after surgery. If you have problems before this, you can contact your doctor or contact the hospital to bring the appointment forward. During this appointment, your symptoms will be reviewed and we will check the wound is healing correctly. The quality of life questionnaire will be checked.
Are there any alternatives to having an autologous sling?
You will have been offered and tried conservative measures, including fluid advice, pelvic floor muscle training, smoking Cessation as well as weight loss, before being offered surgery.
Alternative procedures for stress incontinence of urine include:
- Colposuspension, an operation to support the area around the bladder neck to the back of the bone in the lower tummy.
- Injection of bulking agent at the bladder neck. These can be discussed with your doctor.
The use of Tension-free vaginal tape (TVT) sling was paused in 2017, following safety concerns.
Who can I contact with any queries or concerns?
You should contact your doctor or the hospital if you notice increased temperature, wound swelling and / or pain, smelling wound discharge, blood in your urine or stools, abdominal distension and / or failure to open your bowel.
If you have any problems or questions, please contact.
Princess Royal Hospital, Horsted Keynes Ward: 01444 441881 Extension 5686
Royal Sussex County Hospital, Level 11: 01273 523191 Extension 4013
Urogynaecology Unit at Lewes Victoria Hospital: 01273 474153 Extension 2178
Useful links:
NICE guideline: Urinary incontinence and pelvic organ prolapse in women: management
This patient information leaflet was prepared by Dr. Sharif Ismail, Consultant Subspecialist Urogynaecologist.
This information leaflet has been approved at the Clinical Governance and Safety and Quality Meetings of the Department of Obstetrics and Gynaecology as well as Brighton and Sussex University Hospitals NHS Trust Carer and Patient Information Group (CPIG).
Ratified April 2017 Women’s Safety and Quality Commission.
This leaflet is intended for patients receiving care in Brighton & Hove or Haywards Heath.
The information in this leaflet is for guidance purposes only and is in no way intended to replace professional clinical advice by a qualified practitioner.
Publication Date: May 2021
Review Date: February 2024


